Difference between revisions of "Schwannoma"
m |
|||
| Line 31: | Line 31: | ||
'''Schwannoma''' is a relatively common [[peripheral nerve sheath tumour]]. | '''Schwannoma''' is a relatively common [[peripheral nerve sheath tumour]]. | ||
At the cerebellopontine (CP) angle, they may be referred to as ''acoustic neuroma'' or ''vestibular schwannoma''. | At the [[cerebellopontine angle|cerebellopontine (CP) angle]], they may be referred to as ''acoustic neuroma'' or ''vestibular schwannoma''. | ||
==General== | ==General== | ||
Revision as of 18:55, 30 December 2013
| Schwannoma | |
|---|---|
| Diagnosis in short | |
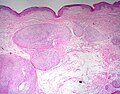
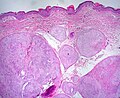
 Schwannoma showing Antoni A and Antoni B areas. HPS stain. | |
|
| |
| LM |
Antoni A areas (cellular, fibrillary, polar, elongated), Antoni B area (pauci-cellular, loose microcystic tissue), Verocay bodies (paucinuclear area surrounded by nuclei), hyaline thickened blood vessels, thick capsule. +/-peripheral lymphoid cuff (esp. GI tract) |
| Subtypes | conventional schwannoma, cellular schwannoma, plexiform schwannoma, melanotic schwannoma |
| LM DDx | meningioma, leiomyoma, GIST, intranodal palisaded myofibroblastoma, MPNST, neurofibroma |
| IHC | S-100 +ve, EMA -ve, CD34 +ve |
| Site | soft tissue - peripheral nerve sheath tumours |
|
| |
| Syndromes | neurofibromatosis type 2, Carney complex (psammomatous melanotic schwannoma) |
|
| |
| Prevalence | common |
| Prognosis | good |
| Clin. DDx | meningioma - esp. at cerebellopontine angle |
Schwannoma is a relatively common peripheral nerve sheath tumour.
At the cerebellopontine (CP) angle, they may be referred to as acoustic neuroma or vestibular schwannoma.
General
- A common neuropathology tumour that occasionally shows-up elsewhere.
- Tumour of tissue surrounding a nerve.
- Axons adjacent to the tumour are normal... but may be compressed.
- May be a part of neurofibromatosis type 2.
Microscopic
Features:[1]
- Antoni A:
- Cellular.
- 'Fibrillary, polar, elongated'.
- Antoni B:
- Pauci-cellular.
- Loose microcystic tissue.
- Verocay bodies - paucinuclear area surrounded by clusters of nuclei - diagnostic feature.
- Hyaline thickened blood vessels.
- Thick capsule.
- In the GI tract: classically have a peripheral lymphoid cuff.[2]
- +/-Hemosiderin deposition within tumour.
Notes:
- Tumour does not smear well.[3]
- Antoni A: may look somewhat like scattered matchsticks.
DDx:
- Meningioma.
- Intranodal palisaded myofibroblastoma - if surrounded by a rim of lymphoid tissue, i.e. intranodal.
- Leiomyoma.
- Gastrointestinal stromal tumour.
- MPNST - schwannoma with ancient change has no significant mitotic activity.[4]
- Neurofibroma.
Images
www:
- Antoni A (pathguy.com).
- Antoni A & Antoni B side-by-side (ajnr.org).
- Cystic schwannoma - several images (upmc.edu).
Schwannoma subtypes
There are four:[5]
- Conventional schwannoma.
- Cellular schwannoma.
- Plexiform schwannoma.
- Melanotic schwannoma.
Conventional schwannoma
- Most common.
Cellular schwannoma
- May mimic MPNST.
Images:
Plexiform schwannoma
- May mimic MPNST if cellular - esp. in childhood.
Images:
Melanotic schwannoma
- May be confused with melanoma.
- Psammomatous form (psammomatous melanotic schwannoma) associated with a heritable disorder (Carney complex).
Note:
- Carney complex:[5]
- Cutaneous lentigines.
- Myxomas (skin (subcutaneous), subcutanous, heart).
- Endocrine neoplasms.
Images:
IHC
Features:[6]
- S-100 +ve.
- Glut1 +ve.
- CD34 +ve.
- Cytokeratins ~70% +ve.[citation needed]
- SOX10 +ve.[7]
- -ve in synovial sarcoma, rhabdomyosarcoma, chondrosarcoma.
- EMA -ve. (???)
- Usually +ve (~75% of the time) in meningiomas.[8]
Others:
Sign out
LESION, LEFT ANTERIOR TIBIA, EXCISION: - SCHWANNOMA. - NEGATIVE FOR MALIGNANCY.
Micro
The sections show a soft tissue spindle cell lesion, with cellular fibrillary areas (Antoni A) and pauci-cellular microcystic areas (Antoni B). There are also pauci-nuclear areas surrounded by clusters of nuclei (Verocay bodies). Thick hyaline blood vessels are present within the lesion. There is no apparent nuclear atypia. Mitotic activity is not readily apparent. No nerve is seen adjacent to the lesion. The lesion is partially encapsulated by fibrous tissue. Focally, ink is seen on the lesional cells.
See also
References
- ↑ Wippold FJ, Lubner M, Perrin RJ, Lämmle M, Perry A (October 2007). "Neuropathology for the neuroradiologist: Antoni A and Antoni B tissue patterns". AJNR Am J Neuroradiol 28 (9): 1633–8. doi:10.3174/ajnr.A0682. PMID 17893219. http://www.ajnr.org/cgi/reprint/28/9/1633.
- ↑ Levy AD, Quiles AM, Miettinen M, Sobin LH (March 2005). "Gastrointestinal schwannomas: CT features with clinicopathologic correlation". AJR Am J Roentgenol 184 (3): 797–802. PMID 15728600. http://www.ajronline.org/cgi/content/full/184/3/797.
- ↑ MUN. 24 November 2010.
- ↑ Chan, PT.; Tripathi, S.; Low, SE.; Robinson, LQ. (2007). "Case report--ancient schwannoma of the scrotum.". BMC Urol 7: 1. doi:10.1186/1471-2490-7-1. PMID 17244372.
- ↑ 5.0 5.1 Kurtkaya-Yapicier O, Scheithauer B, Woodruff JM (July 2003). "The pathobiologic spectrum of Schwannomas". Histol. Histopathol. 18 (3): 925–34. PMID 12792904.
- ↑ Hirose T, Tani T, Shimada T, Ishizawa K, Shimada S, Sano T (April 2003). "Immunohistochemical demonstration of EMA/Glut1-positive perineurial cells and CD34-positive fibroblastic cells in peripheral nerve sheath tumors". Mod. Pathol. 16 (4): 293–8. doi:10.1097/01.MP.0000062654.83617.B7. PMID 12692193. http://www.nature.com/modpathol/journal/v16/n4/full/3880761a.html.
- ↑ Nonaka D, Chiriboga L, Rubin BP (September 2008). "Sox10: a pan-schwannian and melanocytic marker". Am. J. Surg. Pathol. 32 (9): 1291–8. doi:10.1097/PAS.0b013e3181658c14. PMID 18636017.
- ↑ Rushing, EJ.; Bouffard, JP.; McCall, S.; Olsen, C.; Mena, H.; Sandberg, GD.; Thompson, LD. (Jun 2009). "Primary extracranial meningiomas: an analysis of 146 cases.". Head Neck Pathol 3 (2): 116-30. doi:10.1007/s12105-009-0118-1. PMID 19644540.
- ↑ Hasegawa, M.; Muramatsu, N.; Tohma, Y.; Fukaya, K.; Fujisawa, H.; Hayashi, Y.; Tachibana, O.; Kida, S. et al. (Jan 2002). "Expression of E-cadherin-catenin complex in human benign schwannomas.". Histol Histopathol 17 (1): 39-44. PMID 11813884.
- ↑ Carlson, JW.; Fletcher, CD. (Oct 2007). "Immunohistochemistry for beta-catenin in the differential diagnosis of spindle cell lesions: analysis of a series and review of the literature.". Histopathology 51 (4): 509-14. doi:10.1111/j.1365-2559.2007.02794.x. PMID 17711447.