Difference between revisions of "Astrocytoma"
Jump to navigation
Jump to search
(tweak) |
Jensflorian (talk | contribs) (Table with overview) |
||
| Line 1: | Line 1: | ||
An '''astrocytoma''' is a neoplasm derived from an [[neurohistology|astrocyte]]. Astrocytomas are common. This article is a brief introduction them. An overview of CNS tumours is found in the ''[[CNS tumours]]'' article. | An '''astrocytoma''' is a neoplasm derived from an [[neurohistology|astrocyte]]. Astrocytomas are common. This article is a brief introduction them. An overview of CNS tumours is found in the ''[[CNS tumours]]'' article. | ||
=Overview= | |||
{| class="wikitable sortable" | |||
! Name | |||
! Type | |||
! Variants / Patterns | |||
! Image | |||
|- | |||
| Diffuse Astrocytoma, WHO II | |||
| diffuse | |||
| protoplasmatic, fibrillar, gemistocytic | |||
| [[File:Astrocytoma whoII HE.jpg|thumb|center|150px]] | |||
|- | |||
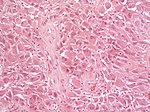
| Anaplastic Astrocytoma, WHO III | |||
| diffuse | |||
| gliomatosis cerebri | |||
| [[File:Anaplastic_astrocytoma_-_very_high_mag.jpg|thumb|center|150px]] | |||
|- | |||
| Glioblastoma, WHO IV | |||
| diffuse | |||
| small cell, epitheloid/rhabdoid, with PNET componet, with granular cell component, giant cell, gliosarcoma | |||
| [[File:Glioblastoma_(1).jpg|thumb|center|150px]] | |||
|- | |||
| Pilocytic astrocytoma, WHO I | |||
| circumscribed | |||
| pilomyxoid astrocytoma, anaplastic pilocytic astrocytoma | |||
| [[File:Rosenthal_HE_40x.jpg|thumb|center|150px]] | |||
|- | |||
| Pleomorphic xanthoastrocytoma, WHO II (PXA) | |||
| circumscribed | |||
| anaplastic PXA | |||
| [[File:PXA_HE_x20.jpg|thumb|center|150px]] | |||
|- | |||
| Subependymal giant cell astrocytoma, WHO I (SEGA) | |||
| circumscribed | |||
| SEGA in tuberous sclerosis | |||
| [[File:SEGA_HE.jpg|thumb|center|150px]] | |||
|} | |||
=Common= | =Common= | ||
==Pilocytic astrocytoma== | ==Pilocytic astrocytoma== | ||
{{Main|Pilocytic astrocytoma}} | {{Main|Pilocytic astrocytoma}} | ||
==Diffuse astrocytoma== | |||
* Grade II and III diffuse astrocytic tumors | |||
* Many of them carry IDH1/2 mutations | |||
==Glioblastoma== | ==Glioblastoma== | ||
| Line 9: | Line 50: | ||
=Uncommon= | =Uncommon= | ||
==Subependymal giant cell astrocytoma== | |||
{{Main|Subependymal giant cell astrocytoma}} | |||
==Pleomorphic xanthroastrocytoma== | ==Pleomorphic xanthroastrocytoma== | ||
*Abbreviated ''PXA''. | *Abbreviated ''PXA''. | ||
| Line 30: | Line 74: | ||
*GFAP +ve -- required for Dx, may be patchy. | *GFAP +ve -- required for Dx, may be patchy. | ||
*S-100 +ve -- cytoplasm, usu. diffuse. | *S-100 +ve -- cytoplasm, usu. diffuse. | ||
==Gliomatosis cerebri== | |||
* Extensively diffusely growing astrocytic neoplasm. | |||
**Currently considered a pattern of diffuse glioma infiltration. | |||
* More than 3 lobes have to be involved, us. bilateral (radiology). | |||
* biologic behaviour corresponds to WHO III (ICD-O: 9381/3) | |||
==H3.3 K27M mutated glioma of the midline== | |||
* High-grade astrocytic neoplasm associated with midline structures | |||
* Mostly in children and adolescents | |||
* Includes diffuse intrinsic pontine gliomas (DPIG) | |||
* Will become provisonal variant in upcoming WHO 2016 classification | |||
* Distinct biological and clinical group with poor prognosis <ref>{{Cite journal | last1 = Khuong-Quang | first1 = DA. | last2 = Buczkowicz | first2 = P. | last3 = Rakopoulos | first3 = P. | last4 = Liu | first4 = XY. | last5 = Fontebasso | first5 = AM. | last6 = Bouffet | first6 = E. | last7 = Bartels | first7 = U. | last8 = Albrecht | first8 = S. | last9 = Schwartzentruber | first9 = J. | title = K27M mutation in histone H3.3 defines clinically and biologically distinct subgroups of pediatric diffuse intrinsic pontine gliomas. | journal = Acta Neuropathol | volume = 124 | issue = 3 | pages = 439-47 | month = Sep | year = 2012 | doi = 10.1007/s00401-012-0998-0 | PMID = 22661320 }}</ref> | |||
==Gliosarcoma== | ==Gliosarcoma== | ||
Revision as of 12:26, 2 July 2015
An astrocytoma is a neoplasm derived from an astrocyte. Astrocytomas are common. This article is a brief introduction them. An overview of CNS tumours is found in the CNS tumours article.
Overview
| Name | Type | Variants / Patterns | Image |
|---|---|---|---|
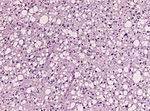
| Diffuse Astrocytoma, WHO II | diffuse | protoplasmatic, fibrillar, gemistocytic | |
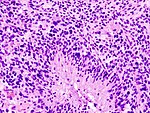
| Anaplastic Astrocytoma, WHO III | diffuse | gliomatosis cerebri | |
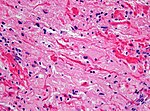
| Glioblastoma, WHO IV | diffuse | small cell, epitheloid/rhabdoid, with PNET componet, with granular cell component, giant cell, gliosarcoma | |
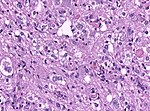
| Pilocytic astrocytoma, WHO I | circumscribed | pilomyxoid astrocytoma, anaplastic pilocytic astrocytoma | |
| Pleomorphic xanthoastrocytoma, WHO II (PXA) | circumscribed | anaplastic PXA | |
| Subependymal giant cell astrocytoma, WHO I (SEGA) | circumscribed | SEGA in tuberous sclerosis |
Common
Pilocytic astrocytoma
Main article: Pilocytic astrocytoma
Diffuse astrocytoma
- Grade II and III diffuse astrocytic tumors
- Many of them carry IDH1/2 mutations
Glioblastoma
Main article: Glioblastoma
Uncommon
Subependymal giant cell astrocytoma
Main article: Subependymal giant cell astrocytoma
Pleomorphic xanthroastrocytoma
- Abbreviated PXA.
General
- Kids & young adults.
- Prognosis usu. good.
Microscopic
Features:
- Large cells with intracytoplasmic lipid accumulation, i.e. foamy cytoplasm - key features.[1]
- May not be obvious/one may have to search for this.
- Focal marked nuclear atypia - including hyperchromasia, marked nuclear enlargement, irregular chromatin.
- Multinucleation - common.
Images:
IHC
Features:[2]
- GFAP +ve -- required for Dx, may be patchy.
- S-100 +ve -- cytoplasm, usu. diffuse.
Gliomatosis cerebri
- Extensively diffusely growing astrocytic neoplasm.
- Currently considered a pattern of diffuse glioma infiltration.
- More than 3 lobes have to be involved, us. bilateral (radiology).
- biologic behaviour corresponds to WHO III (ICD-O: 9381/3)
H3.3 K27M mutated glioma of the midline
- High-grade astrocytic neoplasm associated with midline structures
- Mostly in children and adolescents
- Includes diffuse intrinsic pontine gliomas (DPIG)
- Will become provisonal variant in upcoming WHO 2016 classification
- Distinct biological and clinical group with poor prognosis [3]
Gliosarcoma
General
- Considered to be a variant of glioblastoma by WHO.[4]
- Rare ~ 200 cases reported in the literature.[4]
- Definition: gliosarcoma = glioblastoma + sarcomatous component.[5]
- Usual location (like glioblastoma): temporal lobe.
Microscopic
Features:
- Glioblastoma.
- Sarcomatous component (one of the following):[4][5]
- Fibroblastic.
- Cartilaginous.
- Osseous.
- Smooth muscle.
- Striated muscle.
- Adipocyte.
Images
www:
- Gliosarcoma - several images (upmc.edu).
- Gliosarcoma - case 2 - several images (upmc.edu).
- Gliosarcoma - case 3 - several images (upmc.edu).
IHC
Gliosarcoma with smooth muscle component (gliomyosarcoma):[8]
- SMA +ve.
- Factor VIII +ve.
See also
References
- ↑ URL: http://moon.ouhsc.edu/kfung/jty1/neurotest/Q14-Ans.htm. Accessed on: 13 January 2011.
- ↑ URL: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675%2806%2970469-7. Accessed on: 13 January 2011.
- ↑ Khuong-Quang, DA.; Buczkowicz, P.; Rakopoulos, P.; Liu, XY.; Fontebasso, AM.; Bouffet, E.; Bartels, U.; Albrecht, S. et al. (Sep 2012). "K27M mutation in histone H3.3 defines clinically and biologically distinct subgroups of pediatric diffuse intrinsic pontine gliomas.". Acta Neuropathol 124 (3): 439-47. doi:10.1007/s00401-012-0998-0. PMID 22661320.
- ↑ 4.0 4.1 4.2 Han SJ, Yang I, Tihan T, Prados MD, Parsa AT (February 2010). "Primary gliosarcoma: key clinical and pathologic distinctions from glioblastoma with implications as a unique oncologic entity". J. Neurooncol. 96 (3): 313–20. doi:10.1007/s11060-009-9973-6. PMC 2808523. PMID 19618114. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2808523/.
- ↑ 5.0 5.1 Ayadi L, Charfi S, Khabir A, et al. (March 2010). "[Cerebral gliosarcoma: clinico-pathologic study of 8 cases]" (in French). Tunis Med 88 (3): 142–6. PMID 20415184.
- ↑ Horiguchi, H.; Hirose, T.; Kannuki, S.; Nagahiro, S.; Sano, T. (Aug 1998). "Gliosarcoma: an immunohistochemical, ultrastructural and fluorescence in situ hybridization study.". Pathol Int 48 (8): 595-602. PMID 9736406.
- ↑ URL: http://path.upmc.edu/cases/case361.html. Accessed on: 15 January 2012.
- ↑ Khanna, M.; Siraj, F.; Chopra, P.; Bhalla, S.; Roy, S.. "Gliosarcoma with prominent smooth muscle component (gliomyosarcoma): a report of 10 cases.". Indian J Pathol Microbiol 54 (1): 51-4. doi:10.4103/0377-4929.77324. PMID 21393877.