Difference between revisions of "Celiac sprue"
(→TTG result not available: tweak a bit + add obesity) |
|||
| (3 intermediate revisions by the same user not shown) | |||
| Line 75: | Line 75: | ||
==Microscopic== | ==Microscopic== | ||
Features:<ref name=Ref_PBoD843>{{Ref PBoD|843}}</ref> | Features:<ref name=Ref_PBoD843>{{Ref PBoD|843}}</ref> | ||
*Intraepithelial lymphocytes (IELs) - '''key feature'''. | *[[Intraepithelial lymphocytes]] (IELs) - '''key feature'''. | ||
**Should be more pronounced at tips of villi.<ref name=pmid15280404>{{cite journal |author=Biagi F, Luinetti O, Campanella J, ''et al.'' |title=Intraepithelial lymphocytes in the villous tip: do they indicate potential coeliac disease? |journal=J. Clin. Pathol. |volume=57 |issue=8 |pages=835–9 |year=2004 |month=August |pmid=15280404 |pmc=1770380 |doi=10.1136/jcp.2003.013607 |url=}}</ref> | **Should be more pronounced at tips of villi.<ref name=pmid15280404>{{cite journal |author=Biagi F, Luinetti O, Campanella J, ''et al.'' |title=Intraepithelial lymphocytes in the villous tip: do they indicate potential coeliac disease? |journal=J. Clin. Pathol. |volume=57 |issue=8 |pages=835–9 |year=2004 |month=August |pmid=15280404 |pmc=1770380 |doi=10.1136/jcp.2003.013607 |url=}}</ref> | ||
**Criteria for number varies: | **Criteria for number varies: | ||
| Line 106: | Line 106: | ||
**Super duper rare. | **Super duper rare. | ||
*Drugs - e.g. olmesartan.<ref name=pmid24852741>{{Cite journal | last1 = Fiorucci | first1 = G. | last2 = Puxeddu | first2 = E. | last3 = Colella | first3 = R. | last4 = Paolo Reboldi | first4 = G. | last5 = Villanacci | first5 = V. | last6 = Bassotti | first6 = G. | title = Severe spruelike enteropathy due to olmesartan. | journal = Rev Esp Enferm Dig | volume = 106 | issue = 2 | pages = 142-4 | month = Feb | year = 2014 | doi = | PMID = 24852741 }}</ref> | *Drugs - e.g. olmesartan.<ref name=pmid24852741>{{Cite journal | last1 = Fiorucci | first1 = G. | last2 = Puxeddu | first2 = E. | last3 = Colella | first3 = R. | last4 = Paolo Reboldi | first4 = G. | last5 = Villanacci | first5 = V. | last6 = Bassotti | first6 = G. | title = Severe spruelike enteropathy due to olmesartan. | journal = Rev Esp Enferm Dig | volume = 106 | issue = 2 | pages = 142-4 | month = Feb | year = 2014 | doi = | PMID = 24852741 }}</ref> | ||
*[[obesity|Morbid obesity]].<ref name=pmid17516730>{{Cite journal | last1 = Harpaz | first1 = N. | last2 = Levi | first2 = GS. | last3 = Yurovitsky | first3 = A. | last4 = Kini | first4 = S. | title = Intraepithelial lymphocytosis in architecturally normal small intestinal mucosa: association with morbid obesity. | journal = Arch Pathol Lab Med | volume = 131 | issue = 3 | pages = 344; author reply 344 | month = Mar | year = 2007 | doi = 10.1043/1543-2165(2007)131[344b:IR]2.0.CO;2 | PMID = 17516730 }}</ref> | |||
===Image=== | ===Image=== | ||
| Line 201: | Line 202: | ||
==Sign out== | ==Sign out== | ||
===TTG result not available=== | ===TTG result not available=== | ||
<pre> | |||
Duodenum, Biopsy: | |||
- Small bowel mucosa with increased intraepithelial lymphocytes, villous | |||
architecture and crypt architecture within normal limits, see comment. | |||
- Brunner's glands present. | |||
- NEGATIVE for acute duodenitis. | |||
- NEGATIVE for dysplasia. | |||
Comment: | |||
Focally, there are approximately 50 lymphocytes/100 enterocytes. Increased intraepithelial | |||
lymphocytes is a nonspecific finding that may be seen in a number of conditions, including | |||
infections (e.g. Helicobacter gastritis), obesity, and autoimmune disorders (e.g. Crohn's | |||
disease). It is seen in celiac disease; correlation with serology is suggested, if not done. | |||
</pre> | |||
====Block letters==== | |||
<pre> | <pre> | ||
SMALL BOWEL (DUODENUM), BIOPSY: | SMALL BOWEL (DUODENUM), BIOPSY: | ||
| Line 214: | Line 231: | ||
</pre> | </pre> | ||
====Alternate==== | =====Alternate===== | ||
<pre> | <pre> | ||
DUODENUM, BIOPSY: | DUODENUM, BIOPSY: | ||
Latest revision as of 12:50, 13 June 2019
| Celiac sprue | |
|---|---|
| Diagnosis in short | |
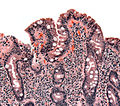
 Celiac disease. H&E stain. | |
|
| |
| Synonyms | celiac disease |
|
| |
| LM | Intraepithelial lymphocytes +/- villous blunting |
| LM DDx | Giardiasis, Enteropathy-associated T-cell lymphoma (EATL), inflammatory bowel disease, MALT lymphoma, others |
| Site | Duodenum |
|
| |
| Associated Dx | dermatitis herpetiformis, IgA deficiency, EATL, duodenal adenocarcinoma |
| Clinical history | improves with gluten free diet |
| Signs | diarrhea |
| Prevalence | uncommon |
| Blood work | TTG elevated (>10 U/mL) |
| Clin. DDx | normal duodenum |
| Treatment | gluten free diet |
Celiac sprue, also celiac disease (abbreviated CD), is a common pathology that affects the duodenum.
It should not be confused with tropical sprue.
An introduction to gastrointestinal pathology is in the gastrointestinal pathology article. It covers basic gastrointestinal histology.
General
- Considered an autoimmune disease.
- The typical individual with celiac disease has a normal weight or is underweight.
Epidemiology
Associated with:
- Dermatitis herpetiformis - skin condition.[2]
- Tx: dapsone.
- IgA deficiency - 10-15X more common in celiac disease vs. healthy controls.[3]
- Risk factor for gastrointestinal T cell lymphoma - known as: enteropathy-associated T cell lymphoma (EATL).
- IgA nephropathy is associated with an increased frequency of celiac disease.[4]
- Esophageal squamous cell carcinoma - increased risk.[5]
- Small bowel adenocarcinoma - increased risk.[6][7]
- Thought to be related to the very rare collagenous sprue - controversial.[8][9]
- Lymphocytic gastritis - seen in ~10% of individuals with celiac disease.[10]
Variants of celiac sprue
- Latent celiac sprue.
- ONLY intraepithelial lymphocytes.
- NO villous arch. change.
- Refractory celiac sprue.
- Subclassified - see microscopic.
- Collagenous sprue.
- Abundant mucosal collagen - see microscopic.
Clinical
Treatment
- Gluten free diet.
- Mnemonic: BROW = barley, rye, oats, wheat.
Serologic testing
- Anti-tissue transglutaminase (TTG) antibody -- >10 U/mL considered positive.[11]
- Alternative test: anti-endomysial antibody.
- Anti-gliadin antibodies.[12]
- IgA deficiency - associated with celiac sprue.
Microscopic
Features:[13]
- Intraepithelial lymphocytes (IELs) - key feature.
- Loss of villi - important feature.
- Normal duodenal biopsy should have 3 good villi.
- Plasma cells - abundant (weak feature).
- Macrophages.
- Mitosis increased (in the crypts).
- +/-Collagen band (pink material in mucosa) - "Collagenous sprue"; must encompass ~25% of mucosa.
Notes:
- If you see acute inflammatory cells, i.e. neutrophils, consider Giardiasis and other infectious etiologies.
- Biopsy should consist of 2-3 sites. In children it is important to sample the duodenal cap, as it is the only affected site in ~10% of cases.
- Flat lesions without IELs are unlikely to be celiac sprue.
- Mucosa erosions are rare in celiac sprue; should prompt consideration of an alternate diagnosis (infection, medications, Crohn's disease).
- Biagi et al.[14] count twenty cells in five (villi) tips.
DDx
- Giardiasis.
- Have giardia organisms.
- Always consider Giardiasis and especially on exams.
- Crohn's disease.
- Helicobacter gastritis.[17]
- Cryptosporidiosis.[17]
- Whipple's disease (very rare).
- Abundant macrophages should make one suspicious.
- Autoimmune enteropathy - pediatric population.
- Super duper rare.
- Drugs - e.g. olmesartan.[18]
- Morbid obesity.[19]
Image
Refractory sprue
- Type I: CD3 ~= CD8.
- Type II: CD3 20% + less than CD8.
Grading
Many pathologists do not grade celiac sprue.
Marsh
The Marsh system, also Marsh-Oberhuber:[15]
| Marsh score | Descriptors | Villi | Intraepithelial lymphocytes (IELs) |
Crypts |
| Normal (Marsh 0) | normal | normal villi | < 40 / 100 epithelial cells | normal crypts |
| Marsh 1 | IELs increased | normal villi | > 40 / 100 epithelial cells | normal crypts |
| Marsh 2 | hypertrophic crypts, IELs | normal villi | > 40 / 100 epithelial cells | hypertrophic crypts |
| Marsh 3a | partial villous atrophy / blunted villi (mild) | mild atrophy | > 40 / 100 epithelial cells | hypertrophic crypts |
| Marsh 3b | moderate-to-marked villous atrophy / blunted villi (moderate-to-marked) |
marked atrophy | > 40 / 100 epithelial cells | hypertrophic crypts |
| Marsh 3c | total villous atrophy, flattened mucosa | absent; flat as a pancake | > 40 / 100 epithelial cells | hypertrophic crypts |
Simplified Marsh/Corazza
A simplified Marsh system - based (only) on villous architecture:[16]
| Grade | Similar Marsh grade | Descriptors | Alternate descriptors |
| A | Marsh 1 | well-formed villi, IELs > 25/100 enterocytes | normal villous architecture |
| B1 | Marsh 3a | partial villous atrophy; villous-crypt ratio < 3:1 | blunted villi |
| B2 | Marsh 3c | total villous atrophy | flattened mucosa |
Notes:
- Villous atrophy can be assessed endoscopically.[20]
IHC
- CD3 -- marks the IELs.[14]
Sign out
TTG result not available
Duodenum, Biopsy: - Small bowel mucosa with increased intraepithelial lymphocytes, villous architecture and crypt architecture within normal limits, see comment. - Brunner's glands present. - NEGATIVE for acute duodenitis. - NEGATIVE for dysplasia. Comment: Focally, there are approximately 50 lymphocytes/100 enterocytes. Increased intraepithelial lymphocytes is a nonspecific finding that may be seen in a number of conditions, including infections (e.g. Helicobacter gastritis), obesity, and autoimmune disorders (e.g. Crohn's disease). It is seen in celiac disease; correlation with serology is suggested, if not done.
Block letters
SMALL BOWEL (DUODENUM), BIOPSY: - SMALL BOWEL MUCOSA WITH INCREASED INTRAEPITHELIAL LYMPHOCYTES, VILLOUS ARCHITECTURE AND CRYPT ARCHITECTURE WITHIN NORMAL LIMITS, SEE COMMENT. - NEGATIVE FOR ACUTE DUODENITIS. - NEGATIVE FOR DYSPLASIA. COMMENT: There are approximately 45 lymphocytes/100 enterocytes. Increased intraepithelial lymphocytes is a nonspecific finding. It is seen in celiac disease; correlation with TTG serology is suggested, if not done.
Alternate
DUODENUM, BIOPSY: - SMALL BOWEL MUCOSA WITH INCREASED INTRAEPITHELIAL LYMPHOCYTES, VILLOUS ARCHITECTURE AND CRYPT ARCHITECTURE WITHIN NORMAL LIMITS, SEE COMMENT. - BRUNNER'S GLANDS PRESENT. - NEGATIVE FOR ACUTE DUODENITIS. - NEGATIVE FOR DYSPLASIA. COMMENT: Focally, there are approximately 50 lymphocytes/100 enterocytes. Increased intraepithelial lymphocytes is a nonspecific finding that may be seen in a number of conditions, including infections (e.g. Helicobacter gastritis), and autoimmune disorders (e.g. Crohn's disease). It is seen in celiac disease; correlation with TTG serology is suggested, if not done.
Positive TTG
DUODENUM, BIOPSY: - SMALL BOWEL MUCOSA WITH BRUNNER'S GLANDS AND AN INCREASE OF INTRAEPITHELIAL LYMPHOCYTES (>50 LYMPHOCYTES/100 ENTEROCYTES), A PRESERVATION OF VILLOUS ARCHITECTURE AND CRYPTS WITHIN NORMAL LIMITS, SEE COMMENT. COMMENT: The findings are consistent with celiac disease, Marsh classification 1.
DUODENUM, BIOPSY: - SMALL BOWEL MUCOSA WITH BRUNNER'S GLANDS, AN INCREASE OF INTRAEPITHELIAL LYMPHOCYTES (>60 LYMPHOCYTES/100 ENTEROCYTES), AND A BLUNTED VILLOUS ARCHITECTURE, SEE COMMENT. COMMENT: The findings are consistent with celiac disease, Marsh classification 3a.
Micro
The sections show small bowel mucosa with Brunner's glands. Increased numbers of intraepithelial lymphocytes are present ~ 50 lymphocytes/100 epithelial cells. The villous architecture is within normal limits (no apparent villous blunting).
Neutrophils are present in the lamina propria; however, they are not found intraepithelial.
The epithelium matures normally to the surface (no dysplasia).
See also
References
- ↑ Singh, I.; Agnihotri, A.; Sharma, A.; Verma, AK.; Das, P.; Thakur, B.; Sreenivas, V.; Gupta, SD. et al. (Feb 2016). "Patients with celiac disease may have normal weight or may even be overweight.". Indian J Gastroenterol. doi:10.1007/s12664-016-0620-9. PMID 26892766.
- ↑ Greenwald, J.; Heng, M. (2007). Toronto Notes for Medical Students 2007 (2007 ed.). The Toronto Notes Inc. for Medical Students Inc.. pp. D22. ISBN 978-0968592878.
- ↑ Kumar, V.; Jarzabek-Chorzelska, M.; Sulej, J.; Karnewska, K.; Farrell, T.; Jablonska, S. (Nov 2002). "Celiac disease and immunoglobulin a deficiency: how effective are the serological methods of diagnosis?". Clin Diagn Lab Immunol 9 (6): 1295-300. PMID 12414763.
- ↑ Smerud, HK.; Fellström, B.; Hällgren, R.; Osagie, S.; Venge, P.; Kristjánsson, G. (Aug 2009). "Gluten sensitivity in patients with IgA nephropathy.". Nephrol Dial Transplant 24 (8): 2476-81. doi:10.1093/ndt/gfp133. PMID 19332868.
- ↑ Messmann, H. (Apr 2001). "Squamous cell cancer of the oesophagus.". Best Pract Res Clin Gastroenterol 15 (2): 249-65. doi:10.1053/bega.2000.0172. PMID 11355914.
- ↑ West, RA.; McNeill, RW. (Dec 1975). "Maxillary alveolar hyperplasia, diagnosis and treatment planning.". J Maxillofac Surg 3 (4): 239-50. PMID 1060711.
- ↑ Rampertab, SD.; Fleischauer, A.; Neugut, AI.; Green, PH. (Aug 2003). "Risk of duodenal adenoma in celiac disease.". Scand J Gastroenterol 38 (8): 831-3. PMID 12940435.
- ↑ Zhao, X.; Johnson, RL. (Jun 2011). "Collagenous sprue: a rare, severe small-bowel malabsorptive disorder.". Arch Pathol Lab Med 135 (6): 803-9. doi:10.1043/2010-0028-RS.1. PMID 21631278.
- ↑ Busto-Bea, V.; Crespo-Pérez, L.; García-Miralles, N.; Ruiz-Del-Árbol-Olmos, L.; Cano-Ruiz, A. (May 2013). "Collagenous sprue: Don´t forget connective tissue in chronic diarrhea evaluation.". Rev Esp Enferm Dig 105 (3): 171-174. PMID 23735026.
- ↑ Feeley, KM.; Heneghan, MA.; Stevens, FM.; McCarthy, CF. (Mar 1998). "Lymphocytic gastritis and coeliac disease: evidence of a positive association.". J Clin Pathol 51 (3): 207-10. PMID 9659261.
- ↑ URL: http://www.mayomedicallaboratories.com/test-catalog/Clinical+and+Interpretive/82587. Accessed on: 13 August 2012.
- ↑ Matthias, T.; Pfeiffer, S.; Selmi, C.; Eric Gershwin, M. (Apr 2010). "Diagnostic challenges in celiac disease and the role of the tissue transglutaminase-neo-epitope.". Clin Rev Allergy Immunol 38 (2-3): 298-301. doi:10.1007/s12016-009-8160-z. PMID 19629760.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 843. ISBN 0-7216-0187-1.
- ↑ 14.0 14.1 14.2 Biagi F, Luinetti O, Campanella J, et al. (August 2004). "Intraepithelial lymphocytes in the villous tip: do they indicate potential coeliac disease?". J. Clin. Pathol. 57 (8): 835–9. doi:10.1136/jcp.2003.013607. PMC 1770380. PMID 15280404. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1770380/.
- ↑ 15.0 15.1 Oberhuber G, Granditsch G, Vogelsang H (October 1999). "The histopathology of coeliac disease: time for a standardized report scheme for pathologists". Eur J Gastroenterol Hepatol 11 (10): 1185–94. PMID 10524652.
- ↑ 16.0 16.1 Corazza GR, Villanacci V, Zambelli C, et al. (July 2007). "Comparison of the interobserver reproducibility with different histologic criteria used in celiac disease". Clin. Gastroenterol. Hepatol. 5 (7): 838–43. doi:10.1016/j.cgh.2007.03.019. PMID 17544877.
- ↑ 17.0 17.1 Brown, I.; Mino-Kenudson, M.; Deshpande, V.; Lauwers, GY. (Jul 2006). "Intraepithelial lymphocytosis in architecturally preserved proximal small intestinal mucosa: an increasing diagnostic problem with a wide differential diagnosis.". Arch Pathol Lab Med 130 (7): 1020-5. doi:10.1043/1543-2165(2006)130[1020:ILIAPP]2.0.CO;2. PMID 16831028.
- ↑ Fiorucci, G.; Puxeddu, E.; Colella, R.; Paolo Reboldi, G.; Villanacci, V.; Bassotti, G. (Feb 2014). "Severe spruelike enteropathy due to olmesartan.". Rev Esp Enferm Dig 106 (2): 142-4. PMID 24852741.
- ↑ Harpaz, N.; Levi, GS.; Yurovitsky, A.; Kini, S. (Mar 2007). "Intraepithelial lymphocytosis in architecturally normal small intestinal mucosa: association with morbid obesity.". Arch Pathol Lab Med 131 (3): 344; author reply 344. doi:10.1043/1543-2165(2007)131[344b:IR]2.0.CO;2. PMID 17516730.
- ↑ Ciaccio EJ, Bhagat G, Tennyson CA, Lewis SK, Hernandez L, Green PH (September 2010). "Quantitative Assessment of Endoscopic Images for Degree of Villous Atrophy in Celiac Disease". Dig Dis Sci. doi:10.1007/s10620-010-1371-6. PMID 20844959.
External links
Review article(s)
- Serra S, Jani PA (November 2006). "An approach to duodenal biopsies". J. Clin. Pathol. 59 (11): 1133–50. doi:10.1136/jcp.2005.031260. PMC 1860495. PMID 16679353. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1860495/?tool=pubmed.