Difference between revisions of "Steatohepatitis"
| (7 intermediate revisions by 2 users not shown) | |||
| Line 6: | Line 6: | ||
| Synonyms = | | Synonyms = | ||
| Micro = [[liver steatosis|steatosis]] (usually macrovesicular); hepatocyte injury -- [[ballooning degeneration]] (key feature), [[Mallory bodies]]; portal bridging (late stage) | | Micro = [[liver steatosis|steatosis]] (usually macrovesicular); hepatocyte injury -- [[ballooning degeneration]] (key feature), [[Mallory bodies]]; portal bridging (late stage) | ||
| Subtypes = by etiology (classically): [[ASH]], [[ | | Subtypes = by etiology (classically): [[ASH]], [[MASH]] -- all almost histologically identical | ||
| LMDDx = [[liver steatosis|steatosis]], [[Wilson disease]], [[hepatitis C]], [[drug-induced liver disease]] | | LMDDx = [[liver steatosis|steatosis]], [[Wilson disease]], [[hepatitis C]], [[drug-induced liver disease]] | ||
| Stains = | | Stains = | ||
| Line 39: | Line 39: | ||
Etiology: | Etiology: | ||
#Alcohol = alcoholic steatohepatitis (ASH). | #Alcohol = alcoholic steatohepatitis (ASH). | ||
# | #Metabolic dysfunction-associated steatohepatitis (MASH). | ||
#*Previously ''non-alcoholic steatohepatitis'' (NASH).<ref name=pmid38692439>{{cite journal |authors=Koda Y, Nagasaki Y |title=Metabolic dysfunction-associated steatohepatitis treated by poly(ethylene glycol)-block-poly(cysteine) block copolymer-based self-assembling antioxidant nanoparticles |journal=J Control Release |volume=370 |issue= |pages=367–378 |date=May 2024 |pmid=38692439 |doi=10.1016/j.jconrel.2024.04.050 |url=}}</ref> | |||
#Drug/toxin.<ref name=pmid12016549>{{Cite journal | last1 = Farrell | first1 = GC. | title = Drugs and steatohepatitis. | journal = Semin Liver Dis | volume = 22 | issue = 2 | pages = 185-94 | month = | year = 2002 | doi = 10.1055/s-2002-30106 | PMID = 12016549 }}</ref> | #Drug/toxin.<ref name=pmid12016549>{{Cite journal | last1 = Farrell | first1 = GC. | title = Drugs and steatohepatitis. | journal = Semin Liver Dis | volume = 22 | issue = 2 | pages = 185-94 | month = | year = 2002 | doi = 10.1055/s-2002-30106 | PMID = 12016549 }}</ref> | ||
| Line 61: | Line 62: | ||
DDx: | DDx: | ||
*[[Steatosis]] - lacks ballooning degeneration. | *[[Steatosis]] - lacks ballooning degeneration and neutrophils. | ||
*[[Wilson disease]]. | *[[Wilson disease]]. | ||
*[[Hepatitis C]]. | *[[Hepatitis C]]. | ||
| Line 172: | Line 173: | ||
====Images==== | ====Images==== | ||
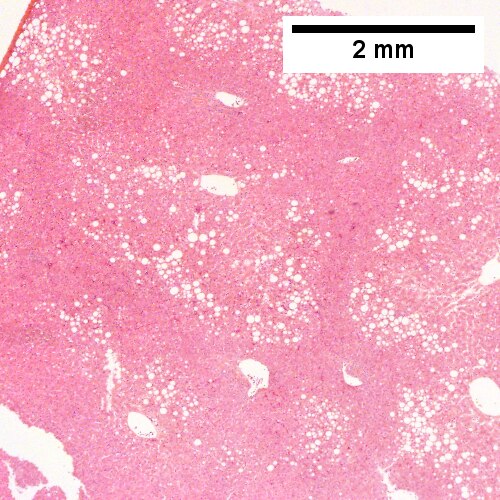
A. [[File:1 Nash 8 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 1. Brunt fibrosis stage 1.]] | |||
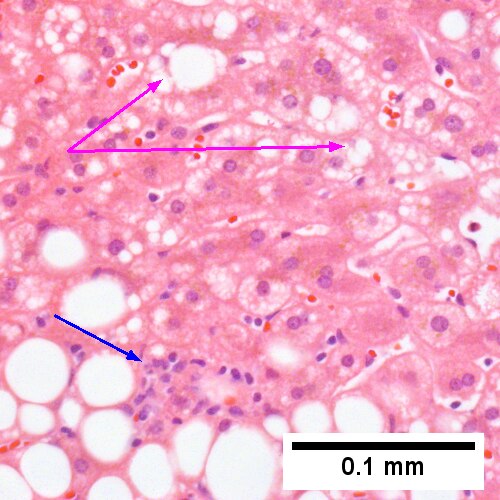
B. [[File:2 Nash 8 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 1. Brunt fibrosis stage 1.]] | |||
<br> | |||
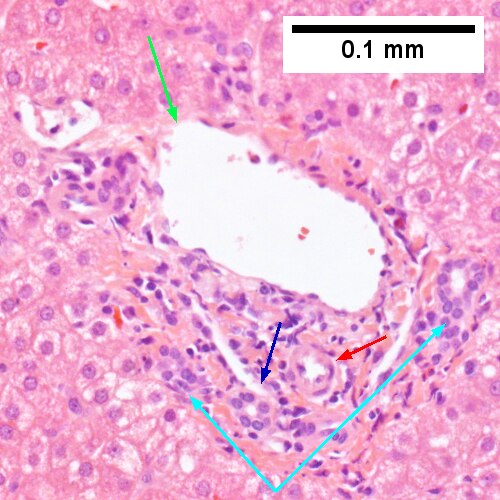
C. [[File:3 Nash 8 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 1. Brunt fibrosis stage 1.]] | |||
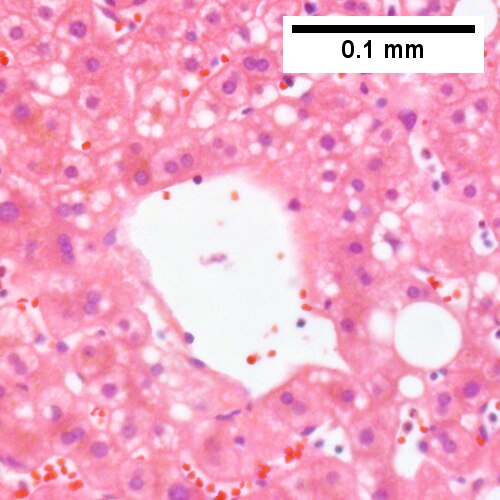
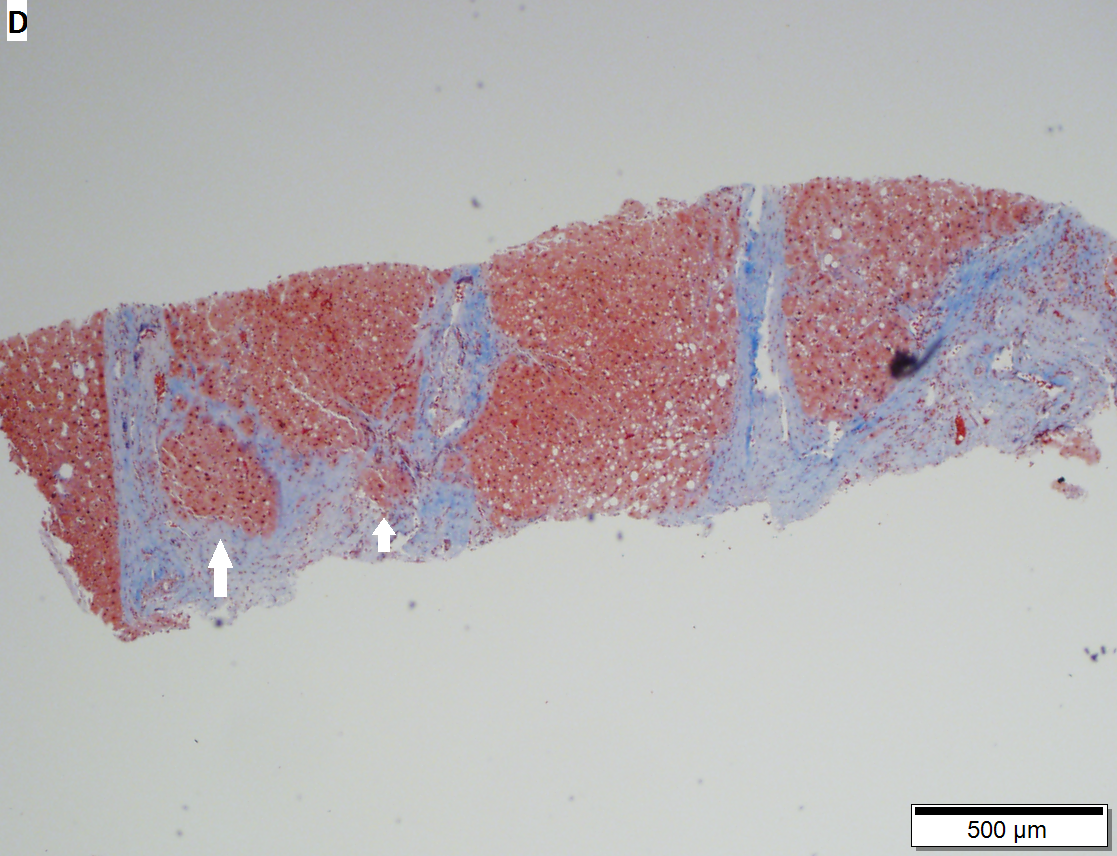
D. [[File:4 Nash 8 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 1. Brunt fibrosis stage 1.]] | |||
<br> | |||
E. [[File:5 Nash 8 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 1. Brunt fibrosis stage 1.]] | |||
F. [[File:6 Nash 8 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 1. Brunt fibrosis stage 1.]] | |||
Steatohepatitis. Brunt necroinflammatory grade 1. Brunt fibrosis stage 1. A. Steatosis afflicts about 30% of hepatocytes; note the absence of visible triads. B. Cytoplasmic tufts of ballooning degeneration [violet arrows] were commonly found; a lymphohistiocytic aggregate [blue arrow], important for NAFLD, but not for Brunt, is seen. C. A triad shows a vein [green arrow], an artery [red arrow], an interlobular duct [blue arrow], and proliferating bile ductules [cyan arrows]; only a few lymphocytes are seen . D. Central vein shows only a few endothelial cells, with somewhat packed hepatocytes surrounding it. E. Trichrome shows mostly space of Disse fibrosis [black arrows], sometimes adjoining hepatocytes [green arrows] show this is a stage 1 fibrosis. F. Trichrome shows a central vein with a minimum of sclerosis; an interhepatocyte fibrous extension [arrow] displays the very beginning of fibrosis. | |||
A. [[File:1 NASH 09 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 2. Brunt fibrosis stage 2.]] | |||
B. [[File:2 NASH 09 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 2. Brunt fibrosis stage 2.]] | |||
<br> | |||
C. [[File:3 NASH 09 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 2. Brunt fibrosis stage 2.]] | |||
D. [[File:4 NASH 09 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 2. Brunt fibrosis stage 2.]] | |||
<br> | |||
E. [[File:5 NASH 09 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 2. Brunt fibrosis stage 2.]] | |||
F. [[File:6 NASH 09 680x512px.tif| Steatohepatitis. Brunt necroinflammatory grade 2. Brunt fibrosis stage 2.]] | |||
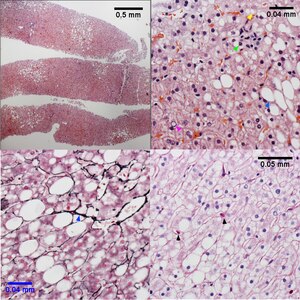
Steatohepatitis. Brunt necroinflammatory grade 2. Brunt fibrosis stage 2. A. Steatosis is not pan-acinar, precluding grade 3. B. Cytoplasmic tufts [arrows] were commonly seen establishing frequent ballooning degeneration of grade 2. C. Trichrome shows periportal fibrosis [arrow] establishing fibrosis stage 2. D. PAS D shows a triad with mild damage, with an interlobular bile duct [green arrow] with luminal sheered epithelium, not neutrophils, a hepatic arteriole [red arrow], a hepatic venule [blue arrow], proliferating bile ductules [cyan arrows]; PAS-D macrophages [black arrows] in triad & sinusoid evidence damage; Neutrophils [magenta arrows] in proliferating bile ductules mean nothing, but in sinusoids indicate damage. E. Reticulin fibers in steatosis afflicted areas can appear abnormally lost, which should not be deemed evidence of hepatocellular carcinoma. F. Reticulin stain here shows hepatocyte acini [arrows], evidence of hepatocellular injury (Row 3 Right 400X). | |||
A. [[File:1 Steatohep 4 680x512px.tif|Panacinar steatosis with unremarkable, small triads (40X).]] | |||
B. [[File:2 Steatohep 4 680x512px.tif|Ballooning degeneration, with cytoplasmic tufts (arrows) (400X).]] | |||
<br> | |||
C. [[File:3 Steatohep 4 680x512px.tif|Lipogranuloma (400X).]] | |||
D. [[File:4 Steatohep 4 680x512px.tif|Triad with mild chronic inflammation without interface hepatitis (400X).]] | |||
Steatohepatitis Brunt necroinflammatory grade 3, Brunt fibrosis stage 1. A. Panacinar steatosis with unremarkable, small triads. B. Ballooning degeneration, with cytoplasmic tufts [arrows]. C. Lipogranuloma. D. Triad with mild chronic inflammation without interface hepatitis. | |||
A. [[File:1 Steatohep 5 680x512px.tif|Steatosis afflicts almost all hepatocytes (pan-acinar) (Row 1 Left 40X).]] | |||
B. [[File:2 Steatohep 5 680x512px.tif|An isolated septal duct with concentric fibrosis (arrow) should not result in a diagnosis of primary sclerosing cholangitis. The patient had a normal bilirubin. (Row 1 Right 200X).]] | |||
<br> | |||
C. [[File:3 Steatohep 5 680x512px.tif|Cytoplasmic tufts (arrows) prove ballooning degeneration (Row 2 Left 400X).]] | |||
D. [[File:4 Steatohep 5 680x512px.tif|PAS with diastase shows PAS-D Kupffer cells (arrows) (Row 2 Right 400X).]] | |||
<br> | |||
E. [[File:5 Steatohep 5 680x512px.tif|Reticulin shows thick black lines (red arrows) of collapse, without portal central bridging. The apparent loss of reticulin due to steatosis (double head cyan arrow) should not be considered regeneration or hepatoma (Row 3 Left 200X).]] | |||
F. [[File:6 Steatohep 5 680x512px.tif|Trichrome shows a bridge (arrows) (Row 3 Right 200X).]] | |||
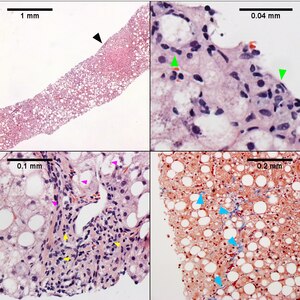
Steatohepatitis. Brunt necroinflammatory grade 3, Brunt fibrosis stage 3. A. Steatosis afflicts almost all hepatocytes (pan-acinar). B. An isolated septal duct with concentric fibrosis [arrow] should not result in a diagnosis of primary sclerosing cholangitis. The woman who underwent the biopsy had a normal bilirubin level, a normal alkaline phosphatase level, and only slightly elevated transaminase levels. C. Cytoplasmic tufts [arrows] prove ballooning degeneration. D. PAS with diastase shows PAS-D Kupffer cells (arrows). E. Reticulin shows thick black lines [red arrows] of collapse, without portal central bridging. The apparent loss of reticulin due to steatosis [double head cyan arrow] should not be considered regeneration or hepatoma. F. Trichrome shows a bridge [arrow]. | |||
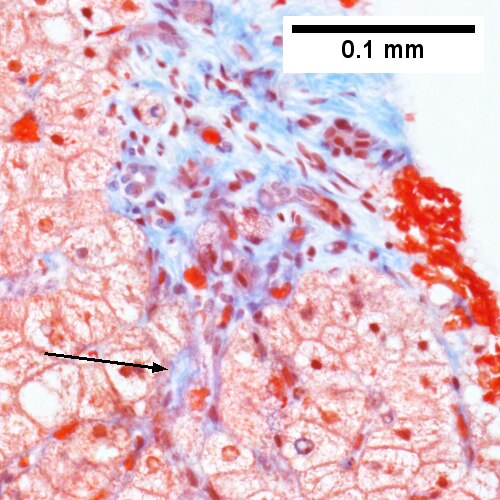
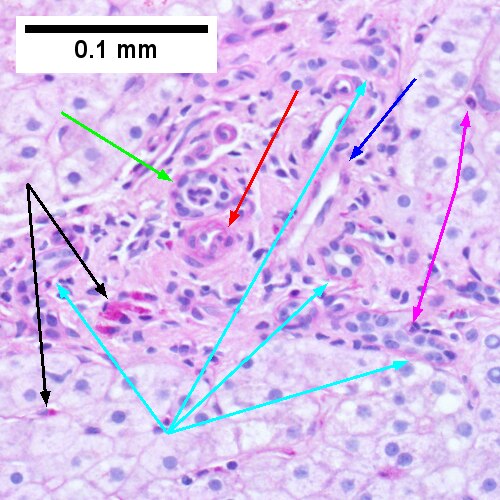
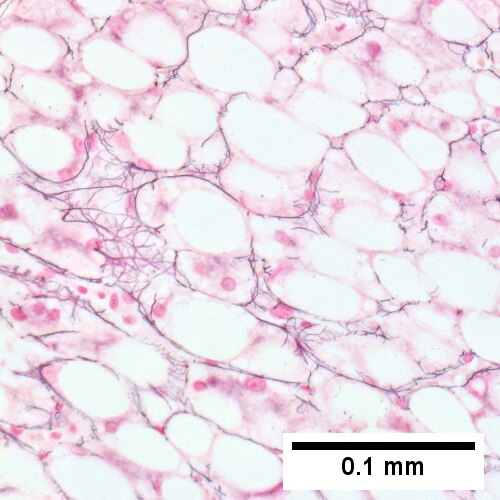
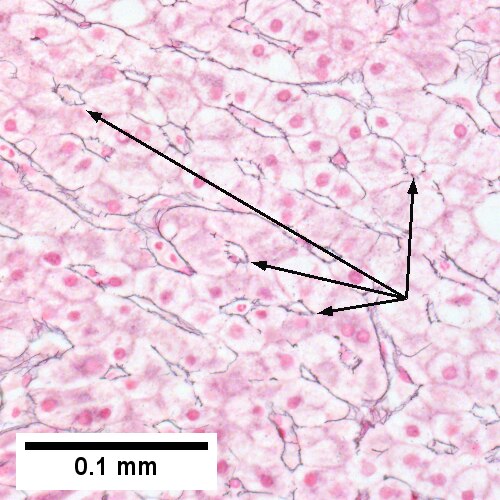
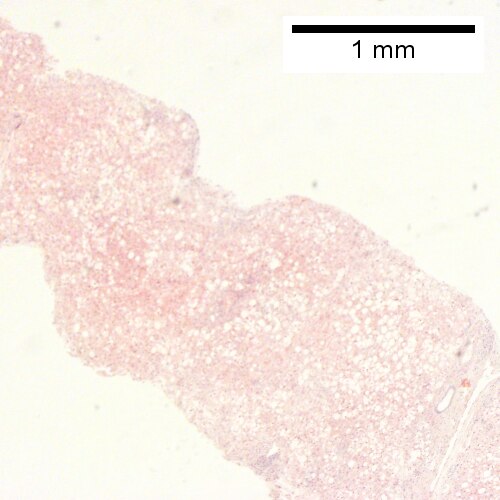
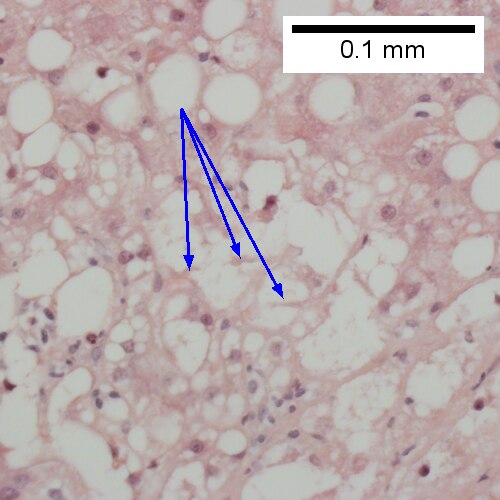
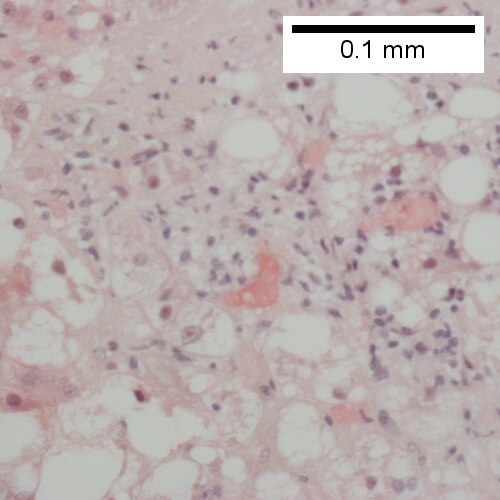
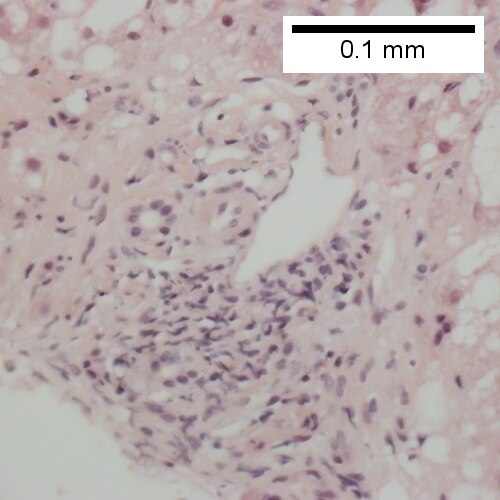
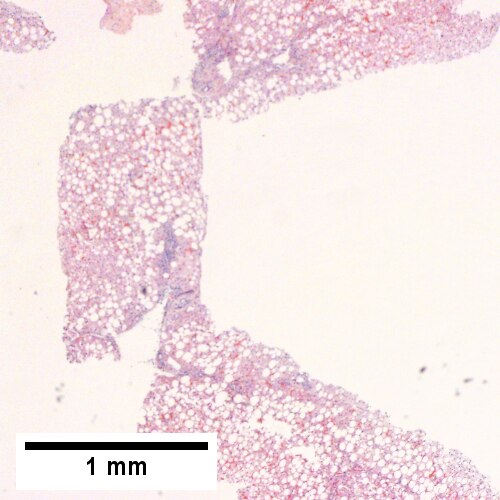
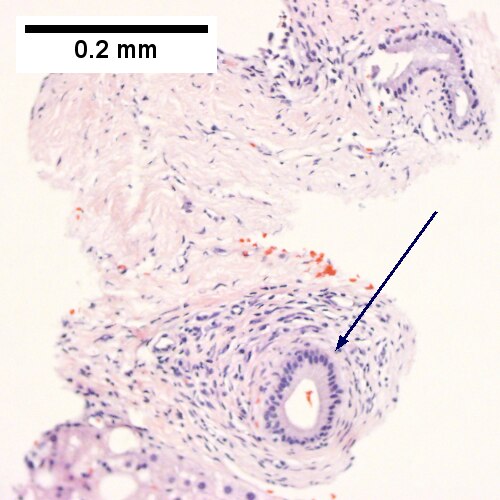
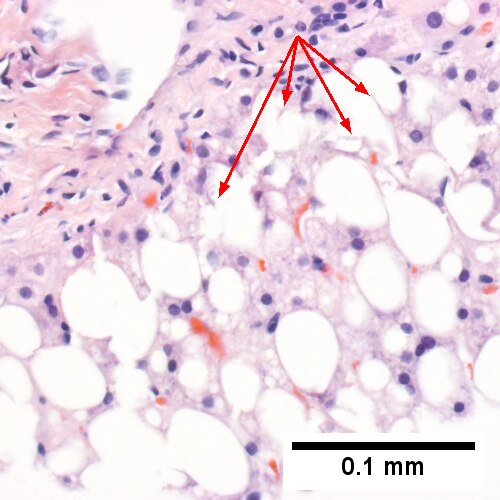
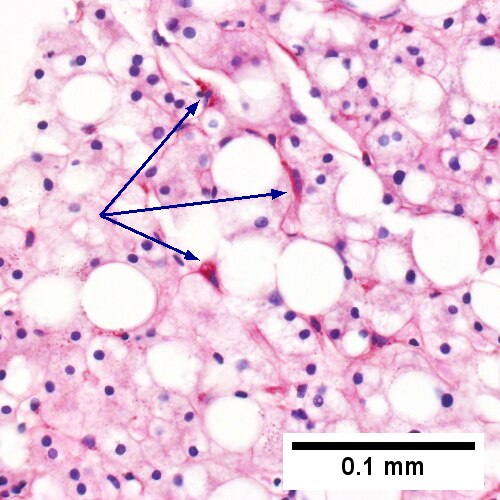
[[File:4 99480485255889 sl 1.png|Cirrhosis with steatohepatitis in a 54 year old man]] | |||
[[File:4 99480485255889 sl 2.png|Cirrhosis with steatohepatitis in a 54 year old man]] | |||
[[File:4 99480485255889 sl 3.png|Cirrhosis with steatohepatitis in a 54 year old man]] | |||
[[File:4 99480485255889 sl 4.png|Cirrhosis with steatohepatitis in a 54 year old man]] | |||
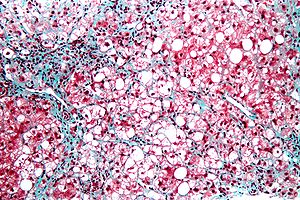
Cirrhosis with steatohepatitis in a 54 year old man with type II diabetes, negative viral serologies, negative alcohol history, negative AMA/ANA, normal ceruloplasmin, low albumin/platelet count, and elevated bilirubin/alkaline phosphatase/transaminase, with hepatosplenomegaly. A. At lower power, no definite triads are seen, but there are potential bands (green arrows) and foci with steatosis (blue arrows). The low percent of hepatocytes afflicted by steatosis would indicate a Brunt necroinflammatory grade 1, here irrelevant as cirrhosis is present. B. Tufts (green arrows) prove ballooning degeneration needed for a diagnosis of steatohepatitis. Foamy macrophage-like hepatocytes (blue arrows) show feathery degeneration is also present. C. Reticulin shows two cell thick cords (green arrows) of regeneration. D. Trichrome shows blue bands and definite nodules (white arrows). At one time, 75% of the biopsy would have had to have been occupied to diagnose cirrhosis. Currently, under the Metavir system, one need only have extensive fibrosis, which would include developing cirrhosis of the HAI system, to obtain a grade IV status, acceptable for transplantation. | |||
{| class="wikitable sortable" | {| class="wikitable sortable" | ||
| [[Image:Steatohepatitis Cases 01.tif |thumb| Fibrosis stage 0 Brunt necroinflammatory grade 1 (WC)]] | | [[Image:Steatohepatitis Cases 01.tif |thumb| Fibrosis stage 0 Brunt necroinflammatory grade 1 (WC)]] | ||
| Line 179: | Line 235: | ||
| [[Image:Steatohepatitis Cases 03.tif |thumb| Fibrosis stage 1 Brunt necroinflammatory grade 2 (WC)]] | | [[Image:Steatohepatitis Cases 03.tif |thumb| Fibrosis stage 1 Brunt necroinflammatory grade 2 (WC)]] | ||
| Necroinflammatory grades Brunt 2, NAH 6. Fibrosis stage 1. About half the hepatocytes show macrovesicular steatosis (UL), with sparing of part of the acinus (UL, Black arrowhead), Lipogranulomas, acomar inflammatory collections, mostly macrophages, about steatosis/ballooning degeneration afflicted hepatocytes or adjacent to them (UR, green arrowheads) are present.Tufts/flocks of ballooning degeneration are readily found (LL, magenta arrowheads). Mild to moderate mononuclear inflammation of portal triads does not exclude steatohepatitis (LL, yellow arrowheads). Trichrome displays the blue thin lines that separate hepatocytes in stage 1 fibrosis (LR blue arrowheads). Original oculars UL 4X, UR 40X (higher pixel photograph), LL 40X , LR 10X | | Necroinflammatory grades Brunt 2, NAH 6. Fibrosis stage 1. About half the hepatocytes show macrovesicular steatosis (UL), with sparing of part of the acinus (UL, Black arrowhead), Lipogranulomas, acomar inflammatory collections, mostly macrophages, about steatosis/ballooning degeneration afflicted hepatocytes or adjacent to them (UR, green arrowheads) are present.Tufts/flocks of ballooning degeneration are readily found (LL, magenta arrowheads). Mild to moderate mononuclear inflammation of portal triads does not exclude steatohepatitis (LL, yellow arrowheads). Trichrome displays the blue thin lines that separate hepatocytes in stage 1 fibrosis (LR blue arrowheads). Original oculars UL 4X, UR 40X (higher pixel photograph), LL 40X , LR 10X | ||
|} | |} | ||
Latest revision as of 19:17, 16 May 2024
| Steatohepatitis | |
|---|---|
| Diagnosis in short | |
 Steatohepatitis. Trichrome stain. | |
|
| |
| LM | steatosis (usually macrovesicular); hepatocyte injury -- ballooning degeneration (key feature), Mallory bodies; portal bridging (late stage) |
| Subtypes | by etiology (classically): ASH, MASH -- all almost histologically identical |
| LM DDx | steatosis, Wilson disease, hepatitis C, drug-induced liver disease |
| Gross | pale/yellowish, often enlarged |
| Site | liver - see medical liver disease |
|
| |
| Associated Dx | obesity, alcohol abuse |
| Prevalence | common |
| Prognosis | dependent on underlying cause |
| Treatment | dependent on underlying cause |
Steatohepatitis is a fatty change of the liver (steaosis) with (histologic) evidence of liver injury. It can be due to a number of different causes.
General
- Steatohepatitis is a label for a set of histopathologic findings.
- Fat accumulation (in hepatocytes) alone is liver steatosis.
- It may be a pattern seen in drug toxicity, e.g. methotrexate toxicity.[1]
Etiology:
- Alcohol = alcoholic steatohepatitis (ASH).
- Metabolic dysfunction-associated steatohepatitis (MASH).
- Previously non-alcoholic steatohepatitis (NASH).[2]
- Drug/toxin.[3]
Notes:
- Pathologists can comment on the etiology; however, the histomorphology is not distinctive. In other words, ASH and NASH are clinical diagnoses.
- Steatohepatitis is a misnomer. It is not an -itis; inflammation is not the (predominant) pathologic process.
Microscopic
Features:
- Steatosis (usually macrovesicular) - key feature.
- If less than 10% ... consider alt. diagnosis/disease process.
- Hepatocyte injury:
- Ballooning degeneration - key feature. †
- Mallory bodies.
- Mallory body wannabes: "occasional cytoplasmic clumping".
- +/-Chicken-wire perisinusoidal fibrosis +/- zone III (centrilobular) fibrosis (early).
- Late-stage disease - portal bridging.[4]
Note:
- † Brunt does not require ballooning to be present to call steatohepatitis;[5] however, a table in a later paper Brunt paper (surveying pathologists) suggest that a significant number of pathologist may consider it a required finding.[6]
DDx:
- Steatosis - lacks ballooning degeneration and neutrophils.
- Wilson disease.
- Hepatitis C.
- Drug-induced liver disease.
Image
Grading steatohepatitis
A simple grading system
| Grade | Characteristics |
|---|---|
| 1 | steatosis, occasional ballooning, scattered PMNs |
| 2 | steatosis, obvious ballooning, obvious PMNs, chronic inflammation |
| 3 | panacinar steatosis, obvious ballooning |
Brunt grading system
Brunt's 1999 paper proposed a system:[5]
| Grade | Steatosis | Neutrophils | Ballooning | Chronic inflammation |
|---|---|---|---|---|
| 1 | <=66% | scattered, rare | occasional or absent (zone 3) | none or mild acinar, none or mild portal |
| 2 | any amount (>33%) | present | obvious ballooning | mild or moderate acinar, mild or moderate portal |
| 3 | panacinar, zone 3 predominant | present | present, obvious | mild acinar inflammation, mild or moderate (not marked) portal |
Clinical Research Network system
Nonalcoholic steatohepatitis Clinical Research Network system for scoring activity - adapted from Brunt and Tiniakos:[7]
| Score | Steatotic hepatocytes (%) |
Foci of lobular lymphocytes |
Ballooning heptocytes |
|---|---|---|---|
| 0 | <5% | none | none |
| 1 | 5-33% | <2 | few |
| 2 | 34%-66% | 2-4 | many |
| 3 | >66% | >4 | (not assigned) |
Staging steatohepatitis
| Stage | Fibrosis | Notes |
|---|---|---|
| 0 | none | - |
| 1 | zone 3 perisinusoidal | may be focal or extensive |
| 2 | perisinusoidal and periportal | no bridging |
| 3 | bridging fibrosis | no nodule formation |
| 4 | nodule formation | - |
Images
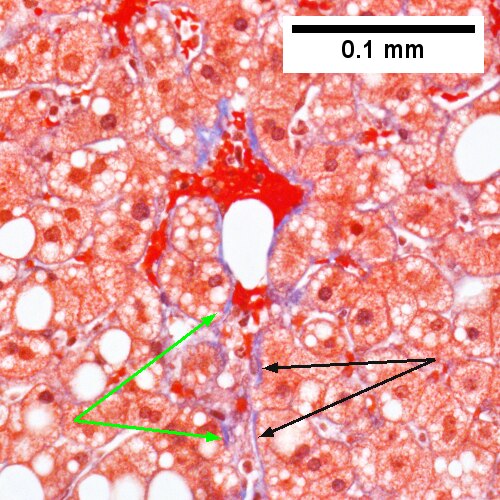
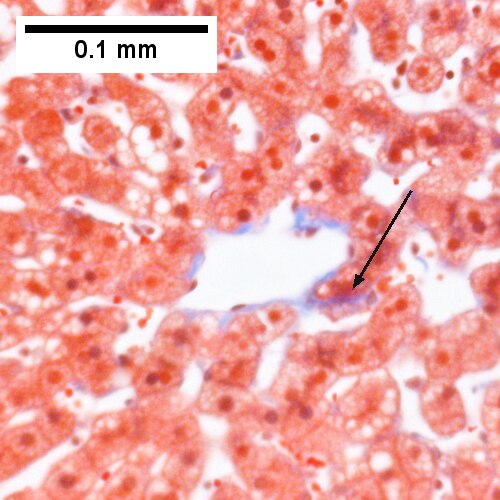
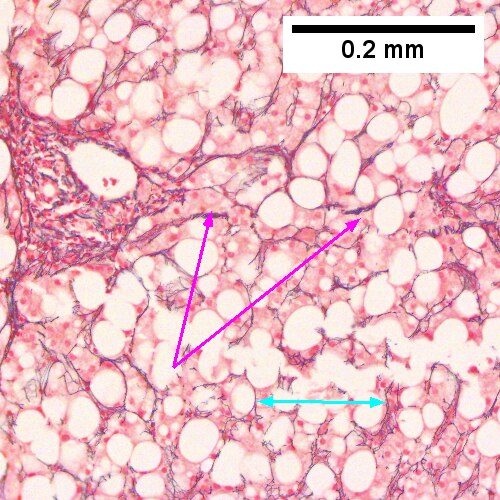
Steatohepatitis. Brunt necroinflammatory grade 1. Brunt fibrosis stage 1. A. Steatosis afflicts about 30% of hepatocytes; note the absence of visible triads. B. Cytoplasmic tufts of ballooning degeneration [violet arrows] were commonly found; a lymphohistiocytic aggregate [blue arrow], important for NAFLD, but not for Brunt, is seen. C. A triad shows a vein [green arrow], an artery [red arrow], an interlobular duct [blue arrow], and proliferating bile ductules [cyan arrows]; only a few lymphocytes are seen . D. Central vein shows only a few endothelial cells, with somewhat packed hepatocytes surrounding it. E. Trichrome shows mostly space of Disse fibrosis [black arrows], sometimes adjoining hepatocytes [green arrows] show this is a stage 1 fibrosis. F. Trichrome shows a central vein with a minimum of sclerosis; an interhepatocyte fibrous extension [arrow] displays the very beginning of fibrosis.
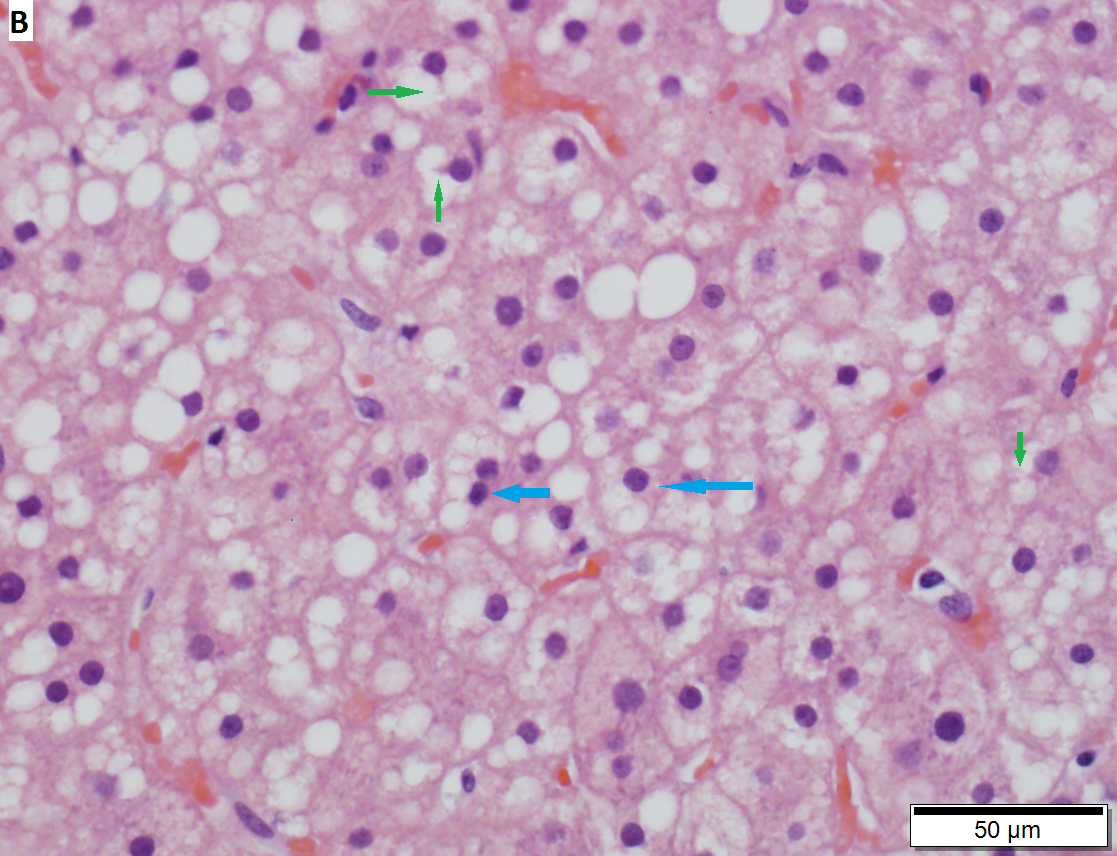
Steatohepatitis. Brunt necroinflammatory grade 2. Brunt fibrosis stage 2. A. Steatosis is not pan-acinar, precluding grade 3. B. Cytoplasmic tufts [arrows] were commonly seen establishing frequent ballooning degeneration of grade 2. C. Trichrome shows periportal fibrosis [arrow] establishing fibrosis stage 2. D. PAS D shows a triad with mild damage, with an interlobular bile duct [green arrow] with luminal sheered epithelium, not neutrophils, a hepatic arteriole [red arrow], a hepatic venule [blue arrow], proliferating bile ductules [cyan arrows]; PAS-D macrophages [black arrows] in triad & sinusoid evidence damage; Neutrophils [magenta arrows] in proliferating bile ductules mean nothing, but in sinusoids indicate damage. E. Reticulin fibers in steatosis afflicted areas can appear abnormally lost, which should not be deemed evidence of hepatocellular carcinoma. F. Reticulin stain here shows hepatocyte acini [arrows], evidence of hepatocellular injury (Row 3 Right 400X).
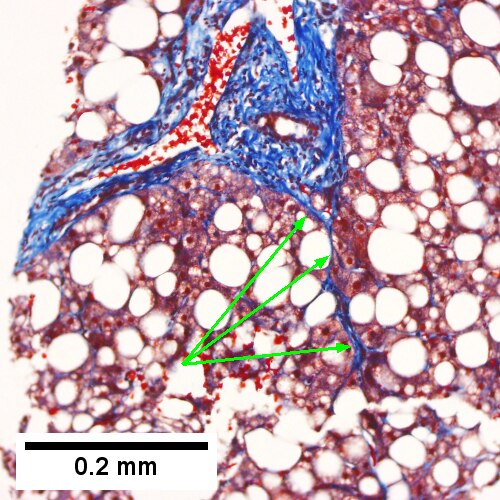
Steatohepatitis Brunt necroinflammatory grade 3, Brunt fibrosis stage 1. A. Panacinar steatosis with unremarkable, small triads. B. Ballooning degeneration, with cytoplasmic tufts [arrows]. C. Lipogranuloma. D. Triad with mild chronic inflammation without interface hepatitis.
Steatohepatitis. Brunt necroinflammatory grade 3, Brunt fibrosis stage 3. A. Steatosis afflicts almost all hepatocytes (pan-acinar). B. An isolated septal duct with concentric fibrosis [arrow] should not result in a diagnosis of primary sclerosing cholangitis. The woman who underwent the biopsy had a normal bilirubin level, a normal alkaline phosphatase level, and only slightly elevated transaminase levels. C. Cytoplasmic tufts [arrows] prove ballooning degeneration. D. PAS with diastase shows PAS-D Kupffer cells (arrows). E. Reticulin shows thick black lines [red arrows] of collapse, without portal central bridging. The apparent loss of reticulin due to steatosis [double head cyan arrow] should not be considered regeneration or hepatoma. F. Trichrome shows a bridge [arrow].
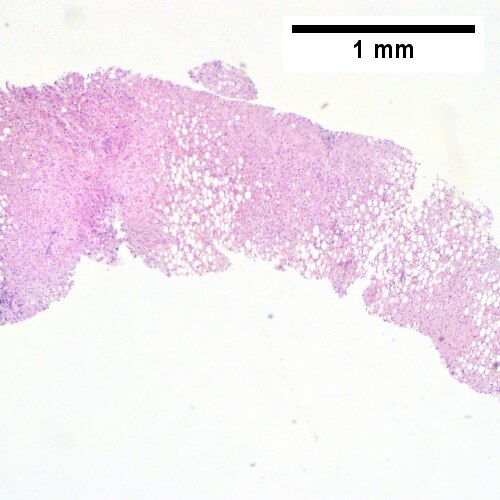
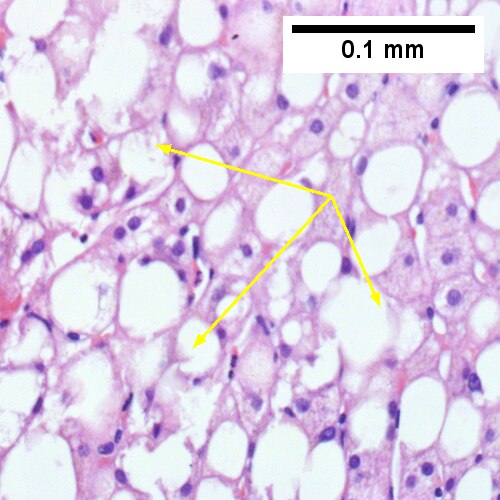
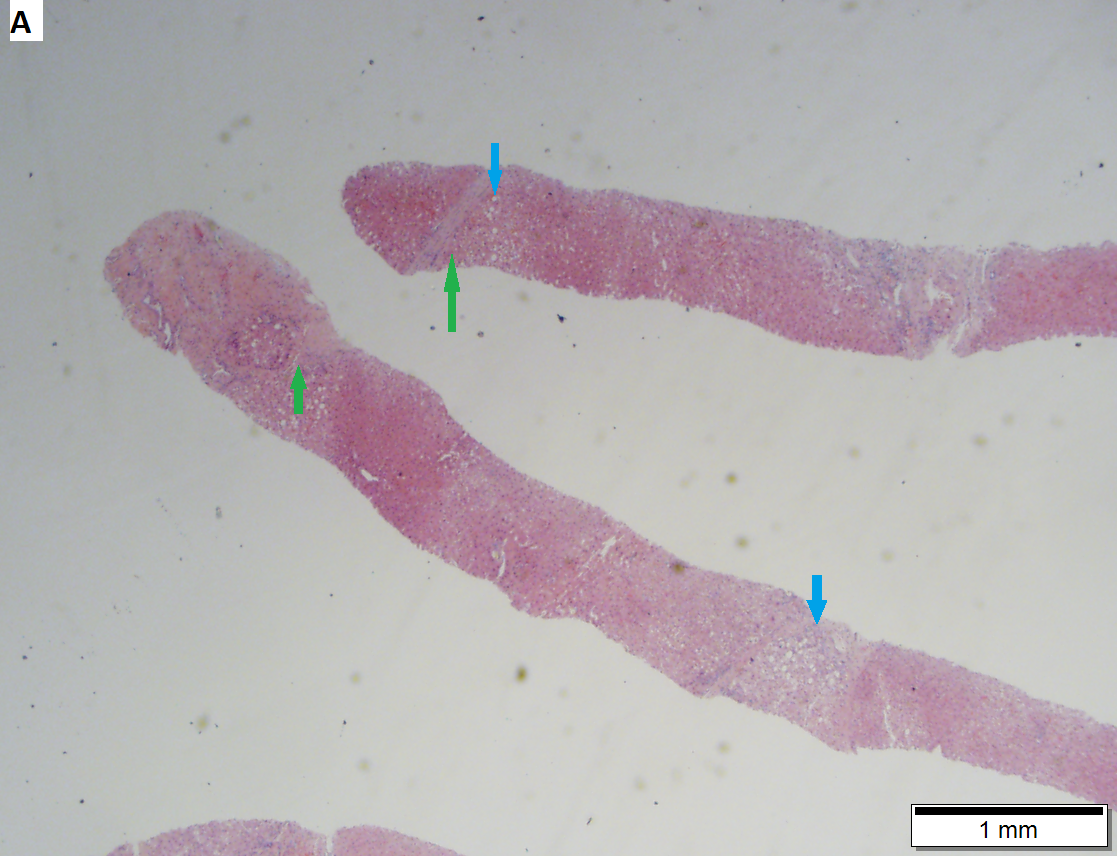
Cirrhosis with steatohepatitis in a 54 year old man with type II diabetes, negative viral serologies, negative alcohol history, negative AMA/ANA, normal ceruloplasmin, low albumin/platelet count, and elevated bilirubin/alkaline phosphatase/transaminase, with hepatosplenomegaly. A. At lower power, no definite triads are seen, but there are potential bands (green arrows) and foci with steatosis (blue arrows). The low percent of hepatocytes afflicted by steatosis would indicate a Brunt necroinflammatory grade 1, here irrelevant as cirrhosis is present. B. Tufts (green arrows) prove ballooning degeneration needed for a diagnosis of steatohepatitis. Foamy macrophage-like hepatocytes (blue arrows) show feathery degeneration is also present. C. Reticulin shows two cell thick cords (green arrows) of regeneration. D. Trichrome shows blue bands and definite nodules (white arrows). At one time, 75% of the biopsy would have had to have been occupied to diagnose cirrhosis. Currently, under the Metavir system, one need only have extensive fibrosis, which would include developing cirrhosis of the HAI system, to obtain a grade IV status, acceptable for transplantation.
| Necroinflammatory grades Brunt 1, NAH 3. Fibrosis stage 0. About 25% of the liver shows steatosis (UL), not pan-acinar. Only rarely identified were either ballooned hepatocytes or inflammatory aggregates. UR shows more macrovesicular (blue arrowhead) than microvesicular (yellow arrowhead) steatosis, with occasional neutrophils in acini ( tip of green arrowhead, benath inflammatory aggregate, with tuft of material in ballooned hepatocyte at base of green arrow), and many glycogenated nuclei (magenta arrowhead). Additional evidence of hepatocellular damage is seen on the reticulin with focal zone III collapse (LL, blue arrowhead) and on the PAS with diastase stain with PAS-D Kupffer cells (LR black arrowheads)
Original oculars. UL 4X. UR 40X, LL 40X, LR 40X | |
| Necroinflammatory grades Brunt 2, NAH 6. Fibrosis stage 1. About half the hepatocytes show macrovesicular steatosis (UL), with sparing of part of the acinus (UL, Black arrowhead), Lipogranulomas, acomar inflammatory collections, mostly macrophages, about steatosis/ballooning degeneration afflicted hepatocytes or adjacent to them (UR, green arrowheads) are present.Tufts/flocks of ballooning degeneration are readily found (LL, magenta arrowheads). Mild to moderate mononuclear inflammation of portal triads does not exclude steatohepatitis (LL, yellow arrowheads). Trichrome displays the blue thin lines that separate hepatocytes in stage 1 fibrosis (LR blue arrowheads). Original oculars UL 4X, UR 40X (higher pixel photograph), LL 40X , LR 10X |
See also
References
- ↑ Schumacher, JD.; Guo, GL. (Nov 2015). "Mechanistic review of drug-induced steatohepatitis.". Toxicol Appl Pharmacol 289 (1): 40-7. doi:10.1016/j.taap.2015.08.022. PMID 26344000.
- ↑ Koda Y, Nagasaki Y (May 2024). "Metabolic dysfunction-associated steatohepatitis treated by poly(ethylene glycol)-block-poly(cysteine) block copolymer-based self-assembling antioxidant nanoparticles". J Control Release 370: 367–378. doi:10.1016/j.jconrel.2024.04.050. PMID 38692439.
- ↑ Farrell, GC. (2002). "Drugs and steatohepatitis.". Semin Liver Dis 22 (2): 185-94. doi:10.1055/s-2002-30106. PMID 12016549.
- ↑ Gramlich, T.; Kleiner, DE.; McCullough, AJ.; Matteoni, CA.; Boparai, N.; Younossi, ZM. (Feb 2004). "Pathologic features associated with fibrosis in nonalcoholic fatty liver disease.". Hum Pathol 35 (2): 196-9. PMID 14991537.
- ↑ 5.0 5.1 Brunt, EM.; Janney, CG.; Di Bisceglie, AM.; Neuschwander-Tetri, BA.; Bacon, BR. (Sep 1999). "Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions.". Am J Gastroenterol 94 (9): 2467-74. doi:10.1111/j.1572-0241.1999.01377.x. PMID 10484010.
- ↑ Brunt, EM. (2001). "Nonalcoholic steatohepatitis: definition and pathology.". Semin Liver Dis 21 (1): 3-16. PMID 11296695.
- ↑ Brunt, EM.; Tiniakos, DG. (Nov 2010). "Histopathology of nonalcoholic fatty liver disease.". World J Gastroenterol 16 (42): 5286-96. PMID 21072891.