Difference between revisions of "Pheochromocytoma"
(→Images) |
|||
| (24 intermediate revisions by 2 users not shown) | |||
| Line 18: | Line 18: | ||
| Assdx = | | Assdx = | ||
| Syndromes = [[Multiple endocrine neoplasia]] 2A and 2B, [[von Hippel-Lindau syndrome]],[[Neurofibromatosis]] type 1, familial paraganglioma syndromes (several) | | Syndromes = [[Multiple endocrine neoplasia]] 2A and 2B, [[von Hippel-Lindau syndrome]],[[Neurofibromatosis]] type 1, familial paraganglioma syndromes (several) | ||
| Clinicalhx = hypertension (classic Hx), paroxysms of tachycardia | | Clinicalhx = hypertension (classic Hx), paroxysms of tachycardia | ||
| Signs = | | Signs = urine metanephrines elevated | ||
| Symptoms = | | Symptoms = headache, anxiety | ||
| Prevalence = uncommon | | Prevalence = uncommon | ||
| Bloodwork = | | Bloodwork = | ||
| Line 38: | Line 38: | ||
Memory device - the rule of 10s:<ref name=Ref_PCPBoD8_586>{{Ref PCPBoD8|586}}</ref> | Memory device - the rule of 10s:<ref name=Ref_PCPBoD8_586>{{Ref PCPBoD8|586}}</ref> | ||
*10% extra-adrenal (e.g. carotid body, | *10% extra-adrenal (e.g. carotid body, ''Organ of Zuckerkandl'' (neighourhood of aortic bifuration/IMA branch point)). | ||
*10% bilateral. | *10% bilateral. | ||
*10% malignant. | *10% malignant. | ||
| Line 71: | Line 71: | ||
*Often haemorrhagic - highly vascular. | *Often haemorrhagic - highly vascular. | ||
*+/-Nuclear pleomorphism. | *+/-Nuclear pleomorphism. | ||
*Rarely pigmented <ref>{{Cite journal | last1 = Bellezza | first1 = G. | last2 = Giansanti | first2 = M. | last3 = Cavaliere | first3 = A. | last4 = Sidoni | first4 = A. | title = Pigmented "black" pheochromocytoma of the adrenal gland: a case report and review of the literature. | journal = Arch Pathol Lab Med | volume = 128 | issue = 10 | pages = e125-8 | month = Oct | year = 2004 | doi = 10.1043/1543-2165(2004)128<e125:PBPOTA>2.0.CO;2 | PMID = 15387689 }}</ref> | |||
Notes: | Notes: | ||
| Line 90: | Line 91: | ||
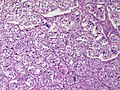
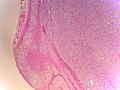
Image:Adrenal Phaeochromocytoma 3 LP CTR.jpg|Adrenal Pheochromocytoma - low power (SKB) | Image:Adrenal Phaeochromocytoma 3 LP CTR.jpg|Adrenal Pheochromocytoma - low power (SKB) | ||
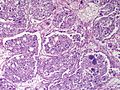
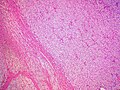
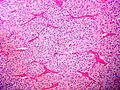
Image:Adrenal Phaeochromocytoma 3 MP CTR.jpg|Adrenal Pheochromocytoma - medium power (SKB) | Image:Adrenal Phaeochromocytoma 3 MP CTR.jpg|Adrenal Pheochromocytoma - medium power (SKB) | ||
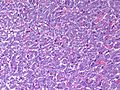
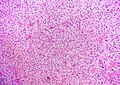
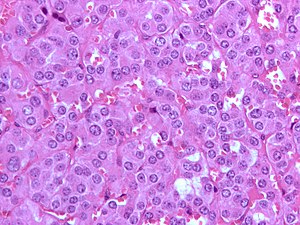
Image:Adrenal Phaeochromocytoma 3 HP CTR.jpg|Adrenal Pheochromocytoma - high power - adrenal cortical neoplasms might be a histologic consideration with this lesion | Image:Adrenal Phaeochromocytoma 3 HP CTR.jpg|Adrenal Pheochromocytoma - high power - version with cleared cells - adrenal cortical neoplasms might be a histologic consideration with this lesion (SKB) | ||
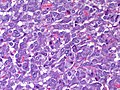
Image:Adrenal Phaeochromocytoma 4 MP CTR.jpg|Pheochromocytoma - medium power (SKB) | Image:Adrenal Phaeochromocytoma 4 MP CTR.jpg|Pheochromocytoma - medium power (SKB) | ||
Image:Adrenal Phaeochromocytoma 4 MP2 CTR.jpg|Pheochromocytoma - medium power (SKB) | Image:Adrenal Phaeochromocytoma 4 MP2 CTR.jpg|Pheochromocytoma - medium power (SKB) | ||
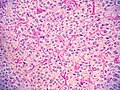
Image:Adrenal Phaeochromocytoma 4 HP CTR.jpg|Adrenal Pheochromocytoma - high power (SKB) | Image:Adrenal Phaeochromocytoma 4 HP CTR.jpg|Adrenal Pheochromocytoma - high power - version with eosinophilic cytoplasm and eosinophilic globules (SKB) | ||
Image:Adrenal Phaeochromocytoma 5 LP PA.JPG|Pheochromocytoma - low power (SKB) | Image:Adrenal Phaeochromocytoma 5 LP PA.JPG|Pheochromocytoma - low power - not a great photo but shows the adrenal cortex pushes aside by the medullary pheochromocytoma (SKB) | ||
Image:Adrenal Phaeochromocytoma 5 MP PA.JPG|Pheochromocytoma - medium power (SKB) | Image:Adrenal Phaeochromocytoma 5 MP PA.JPG|Pheochromocytoma - medium power (SKB) | ||
Image:Adrenal Phaeochromocytoma MP CTR (3).jpg|Pheochromocytoma - medium power (SKB) | |||
Image:Adrenal Phaeochromocytoma MP2 CTR (2).jpg|Pheochromocytoma - medium power (SKB) | |||
Image:Adrenal Phaeochromocytoma HP CTR (2).jpg|Pheochromocytoma - high power - this grey-blue (probably a faded version of the purple blue is also fairly unique to pheochromocytoma (SKB) | |||
Image:Adrenal Phaeochromocytoma 6 MP PA.JPG|Pheochromocytoma - medium power - this pheo is composed of somewhat spindled cells (SKB) | Image:Adrenal Phaeochromocytoma 6 MP PA.JPG|Pheochromocytoma - medium power - this pheo is composed of somewhat spindled cells (SKB) | ||
Image:Adrenal Phaeochromocytoma LP CTR.jpg|Pheochromocytoma - medium power (SKB) | |||
Image:Adrenal Phaeochromocytoma MP CTR.jpg|Pheochromocytoma - medium power (SKB) | Image:Adrenal Phaeochromocytoma MP CTR.jpg|Pheochromocytoma - medium power (SKB) | ||
Image:Adrenal Phaeochromocytoma MP CTR (2).jpg|Pheochromocytoma - medium power (SKB) | Image:Adrenal Phaeochromocytoma MP CTR (2).jpg|Pheochromocytoma - medium power (SKB) | ||
| Line 106: | Line 107: | ||
Image:Adrenal Phaeochromocytoma HP CTR.jpg|Pheochromocytoma - medium power (SKB) | Image:Adrenal Phaeochromocytoma HP CTR.jpg|Pheochromocytoma - medium power (SKB) | ||
Image:Adrenal Pheochromocytoma 4 LP2 PA.JPG|Pheochromocytoma - low power (SKB) | Image:Adrenal Pheochromocytoma 4 LP2 PA.JPG|Pheochromocytoma - low power (SKB) | ||
Image:Adrenal Pheochromocytoma 4 MP2 PA - Copy.JPG|Pheochromocytoma - medium power (SKB) | |||
Image:Adrenal Pheochromocytoma 4 HP2 PA.JPG|Pheochromocytoma - high power (SKB) | Image:Adrenal Pheochromocytoma 4 HP2 PA.JPG|Pheochromocytoma - high power (SKB) | ||
Image:Adrenal Pheochromocytoma LP RBWH.JPG|Pheochromocytoma - low power - shows compressed adrenal cortex to the left (SKB) | |||
Image:Adrenal Pheochromocytoma LP2 RBWH.JPG|Pheochromocytoma - low power (SKB) | |||
Image:Adrenal Pheochromocytoma MP RBWH.JPG|Pheochromocytoma - medium power (SKB) | |||
Image:Adrenal Pheochromocytoma HP RBWH - Copy.JPG|Pheochromocytoma - high power - another with cleared cells (SKB) | |||
Image:Adrenal Pheochromocytoma MP3 RBWH.JPG|Adrenal Pheochromocytoma - medium power (SKB) | |||
Image:Adrenal Pheochromocytoma MP4 RBWH.JPG|Pheochromocytoma - medium power (SKB) | |||
</gallery> | </gallery> | ||
| Line 137: | Line 146: | ||
*Sustentacular cells: | *Sustentacular cells: | ||
**S100 +ve. | **S100 +ve. | ||
Pheochromocytoma versus [[adrenal cortical carcinoma]] (ACC):<ref name=pmid20154585>{{Cite journal | last1 = Sangoi | first1 = AR. | last2 = McKenney | first2 = JK. | title = A tissue microarray-based comparative analysis of novel and traditional immunohistochemical markers in the distinction between adrenal cortical lesions and pheochromocytoma. | journal = Am J Surg Pathol | volume = 34 | issue = 3 | pages = 423-32 | month = Mar | year = 2010 | doi = 10.1097/PAS.0b013e3181cfb506 | PMID = 20154585 }}</ref> | |||
*Melan A -ve. | |||
**Positive in ACC. | |||
*Inhibin -ve. | |||
**Positive in ACC. | |||
*[[Calretinin]] -ve. | |||
**Positive in ACC. | |||
A panel: | |||
*S-100, chromogranin, calretinin, EMA, PAX8. | |||
==[[Electron microscopy]]== | ==[[Electron microscopy]]== | ||
| Line 142: | Line 162: | ||
==Sign out== | ==Sign out== | ||
Mete ''et al.''. created a synoptic report for these cases that may be used.<ref name=pmid24476517>{{cite journal |authors=Mete O, Tischler AS, de Krijger R, McNicol AM, Eisenhofer G, Pacak K, Ezzat S, Asa SL |title=Protocol for the examination of specimens from patients with pheochromocytomas and extra-adrenal paragangliomas |journal=Arch Pathol Lab Med |volume=138 |issue=2 |pages=182–8 |date=February 2014 |pmid=24476517 |pmc=3909881 |doi=10.5858/arpa.2012-0551-OA |url=}}</ref> The ''College of American Pathologists'' does ''not'' have a [[CAP protocols|synoptic]] for these currently (September 2021).{{fact}} | |||
<pre> | |||
Right Adrenal (Mass), Adrenalectomy: | |||
- Pheochromocytoma, margin clear. | |||
Comment: | |||
The tumour stains as follows: | |||
POSITIVE: synaptophysin, chromogranin A, S-100 (sustentacular cells). | |||
NEGATIVE: EMA, inhibin. | |||
Proliferation (Ki-67): <2% of tumour cells. | |||
The immunostaining pattern is consistent with a pheochromocytoma. | |||
</pre> | |||
===Block letters=== | |||
<pre> | <pre> | ||
ADRENAL MASS, RIGHT, ADRENALECTOMY: | ADRENAL MASS, RIGHT, ADRENALECTOMY: | ||
Latest revision as of 15:11, 27 November 2024
| Pheochromocytoma | |
|---|---|
| Diagnosis in short | |
 Pheochromocytoma. H&E stain. | |
|
| |
| LM | Zellballen (nests of cells), fibrovascular septae, salt-and-pepper nuclei, +/-hemorrhage (very common) |
| LM DDx | adrenocortical carcinoma, paraganglioma |
| IHC | chief cells: chromogranin A +ve, synaptophysin +ve; sustentacular cells: S-100 +ve |
| Site | adrenal gland (same tumour arising at other sites known as paraganglioma) |
|
| |
| Syndromes | Multiple endocrine neoplasia 2A and 2B, von Hippel-Lindau syndrome,Neurofibromatosis type 1, familial paraganglioma syndromes (several) |
|
| |
| Clinical history | hypertension (classic Hx), paroxysms of tachycardia |
| Signs | urine metanephrines elevated |
| Symptoms | headache, anxiety |
| Prevalence | uncommon |
| Prognosis | usually benign |
| Clin. DDx | other adrenal gland masses, renal cell carcinoma, other abdominal masses |
Pheochromocytoma is a tumour of the adrenal gland medulla. It may be benign or malignant.
General
- Considered to be a paraganglioma.[1]
- Literally means "dusky" (pheo) "colour" (chromo) - dull appearance on gross.
- Tumour arises from adrenal medulla - chromaffin cells.[2]
Memory device - the rule of 10s:[2]
- 10% extra-adrenal (e.g. carotid body, Organ of Zuckerkandl (neighourhood of aortic bifuration/IMA branch point)).
- 10% bilateral.
- 10% malignant.
- 10% no hypertension.
- 25% associated within a syndrome:
- Multiple endocrine neoplasia 2A and 2B.
- von Hippel-Lindau syndrome.
- Neurofibromatosis type 1.
- Familial paraganglioma syndromes - several - see paraganglioma article.
Clinical
- Classic finding: hypertension.
- Paroxysms (i.e. episodes) of tachycardia, headache, anxiety, hypertension.
Laboratory findings (urine):
- Vanillylmandelic acid (VMA).
- Metanephrines.
Macroscopic
- Medullary tumour
- Round to oval mass
- Dusky red and possibly haemorrhagic
Microscopic
Features:[3]
- Chief cells:
- Usu. polygonal cells, may be spindled.
- Arranged in cell nests - "Zellballen" (literally cell balls) - key feature.
- Stippled chromatin (AKA salt and pepper chromatin) - coarsely granular chromatin.
- Granular cytoplasm, often basophilic - important.
- Sustentacular cells (structural support cell).
- Often haemorrhagic - highly vascular.
- +/-Nuclear pleomorphism.
- Rarely pigmented [4]
Notes:
- The nested architecture (Zellballen) is useful for differentiating from ACC.
- Metastasis sole criteria of malignancy.[2]
- Surrounding adrenal cortex is typically compressed.[5]
DDx:
- Adrenal cortical carcinoma - pheochromocytoma versus adrenal cortical carcinoma.
- Paraganglioma - same lesion arising outside of the adrenal gland.
Images
Pheochromocytoma versus adrenal cortical carcinoma
- Pheochromocytoma and adrenal cortical carcinoma overlap histologically.[6]
Favour pheochromocytoma:
- Small chickenwire-pattern blood vessels, nests, salt-and-pepper chromatin, red blood cell extravasation.
Favour adrenal cortical carcinoma:
- Nucleolus, sheeting.
Malignant pheochromoctyoma
- Robbins (8th Ed.) says metastases are the sole criteria of malignancy.[2]
- Thompson suggests one can differentiate benign from malignant with the aid of the following:[7]
- Marked nuclear atypia.
- Invasion:
- Capsular.
- Vascular.
- Necrosis.
- Cellular monotony.
- Mitoses:
- Rate.
- Atypical mitosis.
IHC
- Chief cells:
- Chromogranin A +ve.
- Synaptophysin +ve.
- Sustentacular cells:
- S100 +ve.
Pheochromocytoma versus adrenal cortical carcinoma (ACC):[6]
- Melan A -ve.
- Positive in ACC.
- Inhibin -ve.
- Positive in ACC.
- Calretinin -ve.
- Positive in ACC.
A panel:
- S-100, chromogranin, calretinin, EMA, PAX8.
Electron microscopy
- Membrane-bound secretory granules.
Sign out
Mete et al.. created a synoptic report for these cases that may be used.[8] The College of American Pathologists does not have a synoptic for these currently (September 2021).[citation needed]
Right Adrenal (Mass), Adrenalectomy:
- Pheochromocytoma, margin clear.
Comment:
The tumour stains as follows:
POSITIVE: synaptophysin, chromogranin A, S-100 (sustentacular cells).
NEGATIVE: EMA, inhibin.
Proliferation (Ki-67): <2% of tumour cells.
The immunostaining pattern is consistent with a pheochromocytoma.
Block letters
ADRENAL MASS, RIGHT, ADRENALECTOMY: - PHEOCHROMOCYTOMA. - SURGICAL MARGIN NEGATIVE FOR PHEOCHROMOCYTOMA. COMMENT: The tumour cells stains for chromogranin and synaptophysin. S-100 marks the sustentacular cells. Inhibin is negative in the tumour cells. The immunostaining pattern is consistent with a pheochromocytoma.
Micro
The sections shows a partially hemorrhagic lesion in the medulla of the adrenal gland that is arranged in nests (Zellballen). The tumour cells have abundant grey/blue granular cytoplasm, and nuclei with granular chromatin (salt and pepper chromatin). The lesion is surrounded by a compressed rim of adrenal cortex and fibrosis tissue. The core of the lesion is fibrotic and has clusters of hemosiderin-laden macrophages.
There is no capsular invasion. Vascular invasion is not identified. There is no necrosis. Mitotic activity is not appreciated.
The adrenal cortex is unremarkable.
See also
References
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 327. ISBN 978-0443066856.
- ↑ 2.0 2.1 2.2 2.3 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 586. ISBN 978-1416054542.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1161. ISBN 978-1416031215.
- ↑ Bellezza, G.; Giansanti, M.; Cavaliere, A.; Sidoni, A. (Oct 2004). "Pigmented "black" pheochromocytoma of the adrenal gland: a case report and review of the literature.". Arch Pathol Lab Med 128 (10): e125-8. doi:10.1043/1543-2165(2004)128<e125:PBPOTA>2.0.CO;2. PMID 15387689.
- ↑ URL: http://www.pathpedia.com/Education/eAtlas/Histopathology/Adrenal/Pheochromocytoma.aspx. Accessed on: 27 May 2013.
- ↑ 6.0 6.1 Sangoi, AR.; McKenney, JK. (Mar 2010). "A tissue microarray-based comparative analysis of novel and traditional immunohistochemical markers in the distinction between adrenal cortical lesions and pheochromocytoma.". Am J Surg Pathol 34 (3): 423-32. doi:10.1097/PAS.0b013e3181cfb506. PMID 20154585.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 259. ISBN 978-0443066856.
- ↑ Mete O, Tischler AS, de Krijger R, McNicol AM, Eisenhofer G, Pacak K, Ezzat S, Asa SL (February 2014). "Protocol for the examination of specimens from patients with pheochromocytomas and extra-adrenal paragangliomas". Arch Pathol Lab Med 138 (2): 182–8. doi:10.5858/arpa.2012-0551-OA. PMC 3909881. PMID 24476517. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3909881/.