Difference between revisions of "Small intestine"
m (→Anatomy) |
(+ileitis) |
||
| (97 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
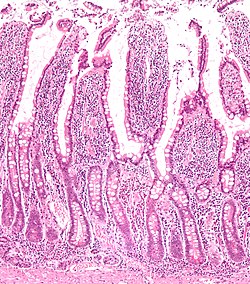
The '''small bowel''' is a relatively well-behaved piece of machinery from the perspective of pathology. It is uncommonly affected by malignancies. | [[Image:Small intestine low mag.jpg|thumb|250px|right|Small bowel mucosa. [[H&E stain]].]] | ||
The '''small intestine''', also '''small bowel''', is a relatively well-behaved piece of machinery from the perspective of [[pathology]]. It is uncommonly affected by malignancies, relative to its length when compared to the [[colon]] and [[rectum]]. | |||
==Anatomy== | =Normal small bowel= | ||
*[[AKA]] ''normal small intestine''. | |||
===Anatomy=== | |||
Consists of three segments: | Consists of three segments: | ||
*Duodenum | *[[Duodenum]] - can be divided into four parts. | ||
*Jejunum. | *Jejunum. | ||
*Ileum. | *Ileum. | ||
| Line 9: | Line 12: | ||
The later two parts keep ''general surgeons'' awake at night (quite literally) 'cause they get obstructed and need urgent operations. | The later two parts keep ''general surgeons'' awake at night (quite literally) 'cause they get obstructed and need urgent operations. | ||
====Length==== | |||
*Normal length of small bowel = 3-8 metres.<ref name=pmid10422101>{{Cite journal | last1 = Nightingale | first1 = JM. | title = Management of patients with a short bowel. | journal = Nutrition | volume = 15 | issue = 7-8 | pages = 633-7 | month = | year = | doi = | PMID = 10422101 }}</ref> | |||
"Short": | |||
* | *Less than 200 cm = ''short bowel syndrome''.<ref name=pmid20709285>{{Cite journal | last1 = Donohoe | first1 = CL. | last2 = Reynolds | first2 = JV. | title = Short bowel syndrome. | journal = Surgeon | volume = 8 | issue = 5 | pages = 270-9 | month = Oct | year = 2010 | doi = 10.1016/j.surge.2010.06.004 | PMID = 20709285 }}</ref><ref name=pmid16207689>{{Cite journal | last1 = Matarese | first1 = LE. | last2 = O'Keefe | first2 = SJ. | last3 = Kandil | first3 = HM. | last4 = Bond | first4 = G. | last5 = Costa | first5 = G. | last6 = Abu-Elmagd | first6 = K. | title = Short bowel syndrome: clinical guidelines for nutrition management. | journal = Nutr Clin Pract | volume = 20 | issue = 5 | pages = 493-502 | month = Oct | year = 2005 | doi = | PMID = 16207689 }}</ref> | ||
**Less than 100 cm usu. requires parenteral nutrition.<ref name=pmid11873098>{{Cite journal | last1 = Sundaram | first1 = A. | last2 = Koutkia | first2 = P. | last3 = Apovian | first3 = CM. | title = Nutritional management of short bowel syndrome in adults. | journal = J Clin Gastroenterol | volume = 34 | issue = 3 | pages = 207-20 | month = Mar | year = 2002 | doi = | PMID = 11873098 }}</ref> | |||
===Histology=== | |||
{{main|Gastrointestinal pathology}} | |||
The ''[[Gastrointestinal pathology]]'' article covers basic histology of the GI tract. | |||
===[[Immunohistochemistry]]=== | |||
*Normal small intestine is CK20 +ve... while adenocarcinoma of the small bowel may be CK20 -ve.<ref>{{cite journal |author=Chen ZM, Wang HL |title=Alteration of cytokeratin 7 and cytokeratin 20 expression profile is uniquely associated with tumorigenesis of primary adenocarcinoma of the small intestine |journal=Am. J. Surg. Pathol. |volume=28 |issue=10 |pages=1352–9 |year=2004 |month=October |pmid=15371952 |doi= |url=}}</ref> | |||
===Sign out=== | |||
<pre> | |||
Small Bowel, Biopsy: | |||
- Small bowel mucosa within normal limits. | |||
</pre> | |||
<pre> | |||
Terminal Ileum, Biopsy: | |||
- Small bowel mucosa within normal limits. | |||
</pre> | |||
<pre> | |||
Terminal Ileum, Biopsy: | |||
- Small bowel mucosa with morphologically benign lymphoid aggregates, negative for significant pathology. | |||
</pre> | |||
====Roux-en-Y gastric bypass==== | |||
{{Main|Obese}} | |||
{{Main|Roux-en-Y gastric bypass}} | |||
== | ====Block letters==== | ||
<pre> | |||
SMALL BOWEL, BIOPSY: | |||
- SMALL BOWEL MUCOSA WITHIN NORMAL LIMITS. | |||
</pre> | |||
<pre> | |||
TERMINAL ILEUM, BIOPSY: | |||
- SMALL BOWEL MUCOSA WITHIN NORMAL LIMITS. | |||
</pre> | |||
<pre> | |||
TERMINAL ILEUM, BIOPSY: | |||
- SMALL BOWEL MUCOSA WITH MORPHOLOGICAL BENIGN LYMPHOID AGGREGATES, NO SIGNIFICANT PATHOLOGY. | |||
</pre> | |||
=The segments= | |||
==Duodenum== | ==Duodenum== | ||
{{main|Duodenum}} | {{main|Duodenum}} | ||
| Line 32: | Line 69: | ||
Common reasons for biopsy: | Common reasons for biopsy: | ||
*Suspected giardia. | *Suspected giardia. | ||
*Suspected celiac sprue. | *Suspected [[celiac sprue]]. | ||
*Is this cancer? | *Is this [[cancer]]? | ||
*Looks normal... want to dot the i's and cross the t's. | *Looks normal... want to dot the i's and cross the t's. | ||
| Line 41: | Line 78: | ||
==Ileum== | ==Ileum== | ||
*This is seen occasionally -- often in the context of IBD and more specifically [[Crohn's disease]]. | *This is seen occasionally -- often in the context of [[IBD]] and more specifically [[Crohn's disease]]. | ||
*Crohn's disease | **[[Crohn's disease]] and[[ulcerative colitis]] are discussed in their respective articles. | ||
=== | =Specific diagnoses= | ||
General | ==Ileitis== | ||
* | :''Active ileitis'' and ''acute ileitis'' redirect here. | ||
* | :This deals with nonspecific ileitis. | ||
* | ===General=== | ||
*Common. | |||
===Microscopic=== | |||
Features: | |||
*Intraepithelial [[neutrophil]]s. | |||
DDx: | |||
*[[Crohn's disease]]. | |||
*Infectious ileitis. | |||
**[[Tuberculosis]]. | |||
*Benign ileum - may have focal intra-epithelial lymphocytes associated with lamina propria lymphoid nodules. | |||
*[[NSAID enteropathy]].<ref name=pmid20532706>{{Cite journal | last1 = Dilauro | first1 = S. | last2 = Crum-Cianflone | first2 = NF. | title = Ileitis: when it is not Crohn's disease. | journal = Curr Gastroenterol Rep | volume = 12 | issue = 4 | pages = 249-58 | month = Aug | year = 2010 | doi = 10.1007/s11894-010-0112-5 | PMID = 20532706 }}</ref> | |||
====Images==== | |||
<gallery> | |||
Image: Mild ileitis -- very low mag.jpg | Ileitis - very low mag. (WC) | |||
Image: Mild ileitis -- low mag.jpg | Ileitis - low mag. (WC) | |||
Image: Mild ileitis -- intermed mag.jpg | Ileitis - intermed. mag. (WC) | |||
Image: Mild ileitis -- high mag.jpg | Ileitis - high mag. (WC) | |||
</gallery> | |||
===Sign out=== | |||
<pre> | |||
Terminal Ileum, Biopsy: | |||
- Small bowel with moderate active inflammation, marked villous blunting, basal plasmacytosis | |||
and prominent eosinophils, see comment. | |||
- NEGATIVE for granulomas. | |||
- NEGATIVE for dysplasia. | |||
Comment: | |||
The inflammation is nonspecific; it could be due to infection, inflammatory bowel disease (especially Crohn's disease), ischemia, or therapy/drugs. Clinical correlation is required. | |||
</pre> | |||
==Small bowel obstruction== | |||
*Abbreviated ''SBO''. | |||
{{Main|Small bowel obstruction}} | |||
==Small bowel neoplasms== | ==Small bowel neoplasms== | ||
*Adenocarcinoma - like colonic. | *Adenocarcinoma - like colonic. | ||
*Adenosquamous carcinoma. | *[[Adenosquamous carcinoma]]. | ||
* | *[[Neuroendocrine tumour]]. | ||
*[[GIST]]. | *[[GIST]]. | ||
*Schwannoma. | *[[Schwannoma]]. | ||
**Classically have a ''peripheral lymphoid cuff''.<ref name=pmid15728600>{{cite journal |author=Levy AD, Quiles AM, Miettinen M, Sobin LH |title=Gastrointestinal schwannomas: CT features with clinicopathologic correlation |journal=AJR Am J Roentgenol |volume=184 |issue=3 |pages=797–802 |year=2005 |month=March |pmid=15728600 |doi= |url=http://www.ajronline.org/cgi/content/full/184/3/797}}</ref> | |||
==Mechanical small bowel perforation== | |||
:See ''[[mechanical bowel perforation]]''. | |||
==Ileal nodular lymphoid hyperplasia== | |||
*[[AKA]] ''nodular lymphoid hyperplasia of the terminal ileum''. | |||
===General=== | |||
*An uncommon diagnosis. | |||
*May be associated with hypogammaglobulinemia.<ref name=pmid8782302>{{cite journal |author=Yamaue H, Tanimura H, Ishimoto K, Morikawa Y, Kakudo K |title=Nodular lymphoid hyperplasia of the terminal ileum: report of a case and the findings of an immunological analysis |journal=Surg. Today |volume=26 |issue=6 |pages=431-4 |year=1996 |pmid=8782302 |doi= |url=}}</ref> | |||
===Gross=== | |||
*Mucosal nodularity. | |||
===Microscopic=== | |||
Features: | |||
*Lymphoid nodules +/- germinal centre formation. | |||
Note: | |||
*Tingible body macrophages suggest an aggregate is benign. | |||
DDx: | |||
*[[MALT lymphoma]]. | |||
*[[Mantle cell lymphoma]]. | |||
*Other lymphomas. | |||
===IHC=== | |||
*[[CD20]] and CD3 - mixed population of lymphocytes. | |||
*[[CD23]] - follicular dendritic cells. | |||
*Cyclin D1 -ve. | |||
Note: | |||
*IHC should be used if there is: | |||
**Clinical suspicion. | |||
**Histologic suspicion - either: | |||
***Sheets of lymphocytes without apparent germinal centre formation in a larger area (~ 2 mm). | |||
***[[Lymphoepithelial lesion]]s. | |||
===Sign out=== | |||
<pre> | |||
TERMINAL ILEUM, BIOPSY: | |||
- SMALL BOWEL MUCOSA WITH LYMPHOID NODULES WITH GERMINAL CENTRE | |||
FORMATION -- NO SIGNIFICANT PATHOLOGY. | |||
- NEGATIVE FOR ILEITIS. | |||
</pre> | |||
<pre> | |||
TERMINAL ILEUM, BIOPSY: | |||
- SMALL BOWEL MUCOSA WITH LYMPHOID HYPERPLASIA -- NO SIGNIFICANT PATHOLOGY. | |||
</pre> | |||
====Micro==== | |||
The sections show small bowel mucosa with lymphoid hyperplasia. | |||
Immunostains for CD3 and CD20 show a mixed population of lymphocytes. A CD23 immunostain shows follicular dendritic cell networks. A cyclin D1 immunostain is negative. | |||
=====Alternate===== | |||
Immunostains for CD3 and CD20 show a mixed population of lymphocytes, with CD20 cells predominating. A cyclin D1 immunostain is negative. A CD23 immunostain shows follicular dendritic cell networks. | |||
==Multiple lymphomatous polyposis== | |||
*Abbreviated ''MLP''. | |||
*[[AKA]] ''lymphomatous polyposis''. | |||
===General=== | |||
*MLP is classically due to ''[[mantle cell lymphoma]]''.<ref name=pmid20206107>{{Cite journal | last1 = Ruskoné-Fourmestraux | first1 = A. | last2 = Audouin | first2 = J. | title = Primary gastrointestinal tract mantle cell lymphoma as multiple lymphomatous polyposis. | journal = Best Pract Res Clin Gastroenterol | volume = 24 | issue = 1 | pages = 35-42 | month = Feb | year = 2010 | doi = 10.1016/j.bpg.2009.12.001 | PMID = 20206107 }}</ref> | |||
**May be due to other lymphomas, e.g. [[follicular lymphoma]].<ref>URL: [http://www.pathmax.com/gilymph.html http://www.pathmax.com/gilymph.html]. Accessed on: 1 April 2012.</ref> | |||
===Microscopic=== | |||
Features: | |||
*Lymphoid nodules consisting of (small) atypical lymphocytes with an abnormal architecture. | |||
===IHC=== | |||
See ''[[small cell lymphomas]]''. | |||
==Small bowel diaphragm disease== | |||
*[[AKA]] ''diaphragm disease''. | |||
===General=== | |||
*Strictures associated with chronic [[NSAID]] use.<ref name=pmid1481311>{{cite journal |author=McCune KH, Allen D, Cranley B |title=Small bowel diaphragm disease--strictures associated with non-steroidal anti-inflammatory drugs |journal=Ulster Med J |volume=61 |issue=2 |pages=182–4 |year=1992 |month=October |pmid=1481311 |pmc=2448949 |doi= |url=}}</ref> | |||
*Usu. mid to distal ileum. | |||
===Microscopic=== | |||
Features:<ref name=pmid1481311/> | |||
*Focal submucosal fibrosis. | |||
**+/-Distortion of adjacent muscularis propria. | |||
**+/-Adjacent mucosal erosions/granulation tissue. | |||
DDx: | |||
*Cryptogenic multifocal ulcerous stenosing enteritis.<ref>{{Cite journal | last1 = Chung | first1 = SH. | last2 = Jo | first2 = Y. | last3 = Ryu | first3 = SR. | last4 = Ahn | first4 = SB. | last5 = Son | first5 = BK. | last6 = Kim | first6 = SH. | last7 = Park | first7 = YS. | last8 = Hong | first8 = YO. | title = Diaphragm disease compared with cryptogenic multifocal ulcerous stenosing enteritis. | journal = World J Gastroenterol | volume = 17 | issue = 23 | pages = 2873-6 | month = Jun | year = 2011 | doi = 10.3748/wjg.v17.i23.2873 | PMID = 21734797 }}</ref> (???) | |||
*[[Crohn's disease]]. | |||
==Meckel diverticulum== | |||
{{Main|Meckel diverticulum}} | |||
==Ischemic enteritis== | |||
{{Main|Ischemic enteritis}} | |||
=Weird stuff= | |||
==Autoimmune enteropathy== | |||
*Abbreviated as ''AIE''. | |||
{{Main|Autoimmune enteropathy}} | |||
=See also= | |||
*[[Stomach]]. | *[[Stomach]]. | ||
*[[Gastrointestinal pathology]]. | *[[Gastrointestinal pathology]]. | ||
*[[Colon]]. | *[[Colon]]. | ||
=References= | |||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Gastrointestinal pathology]] | [[Category:Gastrointestinal pathology]] | ||
Latest revision as of 16:07, 18 November 2022
The small intestine, also small bowel, is a relatively well-behaved piece of machinery from the perspective of pathology. It is uncommonly affected by malignancies, relative to its length when compared to the colon and rectum.
Normal small bowel
- AKA normal small intestine.
Anatomy
Consists of three segments:
- Duodenum - can be divided into four parts.
- Jejunum.
- Ileum.
The later two parts keep general surgeons awake at night (quite literally) 'cause they get obstructed and need urgent operations.
Length
- Normal length of small bowel = 3-8 metres.[1]
"Short":
- Less than 200 cm = short bowel syndrome.[2][3]
- Less than 100 cm usu. requires parenteral nutrition.[4]
Histology
The Gastrointestinal pathology article covers basic histology of the GI tract.
Immunohistochemistry
- Normal small intestine is CK20 +ve... while adenocarcinoma of the small bowel may be CK20 -ve.[5]
Sign out
Small Bowel, Biopsy: - Small bowel mucosa within normal limits.
Terminal Ileum, Biopsy: - Small bowel mucosa within normal limits.
Terminal Ileum, Biopsy: - Small bowel mucosa with morphologically benign lymphoid aggregates, negative for significant pathology.
Roux-en-Y gastric bypass
Block letters
SMALL BOWEL, BIOPSY: - SMALL BOWEL MUCOSA WITHIN NORMAL LIMITS.
TERMINAL ILEUM, BIOPSY: - SMALL BOWEL MUCOSA WITHIN NORMAL LIMITS.
TERMINAL ILEUM, BIOPSY: - SMALL BOWEL MUCOSA WITH MORPHOLOGICAL BENIGN LYMPHOID AGGREGATES, NO SIGNIFICANT PATHOLOGY.
The segments
Duodenum
The duodenum is often biopsied by gastroenterologists.
Common reasons for biopsy:
- Suspected giardia.
- Suspected celiac sprue.
- Is this cancer?
- Looks normal... want to dot the i's and cross the t's.
Jejunum
- Uncommonly seen by pathologists.
- May be seen in the context of a resection done for a bowel obstruction.
Ileum
- This is seen occasionally -- often in the context of IBD and more specifically Crohn's disease.
- Crohn's disease andulcerative colitis are discussed in their respective articles.
Specific diagnoses
Ileitis
- Active ileitis and acute ileitis redirect here.
- This deals with nonspecific ileitis.
General
- Common.
Microscopic
Features:
- Intraepithelial neutrophils.
DDx:
- Crohn's disease.
- Infectious ileitis.
- Benign ileum - may have focal intra-epithelial lymphocytes associated with lamina propria lymphoid nodules.
- NSAID enteropathy.[6]
Images
Sign out
Terminal Ileum, Biopsy: - Small bowel with moderate active inflammation, marked villous blunting, basal plasmacytosis and prominent eosinophils, see comment. - NEGATIVE for granulomas. - NEGATIVE for dysplasia. Comment: The inflammation is nonspecific; it could be due to infection, inflammatory bowel disease (especially Crohn's disease), ischemia, or therapy/drugs. Clinical correlation is required.
Small bowel obstruction
- Abbreviated SBO.
Small bowel neoplasms
- Adenocarcinoma - like colonic.
- Adenosquamous carcinoma.
- Neuroendocrine tumour.
- GIST.
- Schwannoma.
- Classically have a peripheral lymphoid cuff.[7]
Mechanical small bowel perforation
Ileal nodular lymphoid hyperplasia
- AKA nodular lymphoid hyperplasia of the terminal ileum.
General
- An uncommon diagnosis.
- May be associated with hypogammaglobulinemia.[8]
Gross
- Mucosal nodularity.
Microscopic
Features:
- Lymphoid nodules +/- germinal centre formation.
Note:
- Tingible body macrophages suggest an aggregate is benign.
DDx:
- MALT lymphoma.
- Mantle cell lymphoma.
- Other lymphomas.
IHC
Note:
- IHC should be used if there is:
- Clinical suspicion.
- Histologic suspicion - either:
- Sheets of lymphocytes without apparent germinal centre formation in a larger area (~ 2 mm).
- Lymphoepithelial lesions.
Sign out
TERMINAL ILEUM, BIOPSY: - SMALL BOWEL MUCOSA WITH LYMPHOID NODULES WITH GERMINAL CENTRE FORMATION -- NO SIGNIFICANT PATHOLOGY. - NEGATIVE FOR ILEITIS.
TERMINAL ILEUM, BIOPSY: - SMALL BOWEL MUCOSA WITH LYMPHOID HYPERPLASIA -- NO SIGNIFICANT PATHOLOGY.
Micro
The sections show small bowel mucosa with lymphoid hyperplasia.
Immunostains for CD3 and CD20 show a mixed population of lymphocytes. A CD23 immunostain shows follicular dendritic cell networks. A cyclin D1 immunostain is negative.
Alternate
Immunostains for CD3 and CD20 show a mixed population of lymphocytes, with CD20 cells predominating. A cyclin D1 immunostain is negative. A CD23 immunostain shows follicular dendritic cell networks.
Multiple lymphomatous polyposis
- Abbreviated MLP.
- AKA lymphomatous polyposis.
General
- MLP is classically due to mantle cell lymphoma.[9]
- May be due to other lymphomas, e.g. follicular lymphoma.[10]
Microscopic
Features:
- Lymphoid nodules consisting of (small) atypical lymphocytes with an abnormal architecture.
IHC
See small cell lymphomas.
Small bowel diaphragm disease
- AKA diaphragm disease.
General
Microscopic
Features:[11]
- Focal submucosal fibrosis.
- +/-Distortion of adjacent muscularis propria.
- +/-Adjacent mucosal erosions/granulation tissue.
DDx:
- Cryptogenic multifocal ulcerous stenosing enteritis.[12] (???)
- Crohn's disease.
Meckel diverticulum
Ischemic enteritis
Weird stuff
Autoimmune enteropathy
- Abbreviated as AIE.
See also
References
- ↑ Nightingale, JM.. "Management of patients with a short bowel.". Nutrition 15 (7-8): 633-7. PMID 10422101.
- ↑ Donohoe, CL.; Reynolds, JV. (Oct 2010). "Short bowel syndrome.". Surgeon 8 (5): 270-9. doi:10.1016/j.surge.2010.06.004. PMID 20709285.
- ↑ Matarese, LE.; O'Keefe, SJ.; Kandil, HM.; Bond, G.; Costa, G.; Abu-Elmagd, K. (Oct 2005). "Short bowel syndrome: clinical guidelines for nutrition management.". Nutr Clin Pract 20 (5): 493-502. PMID 16207689.
- ↑ Sundaram, A.; Koutkia, P.; Apovian, CM. (Mar 2002). "Nutritional management of short bowel syndrome in adults.". J Clin Gastroenterol 34 (3): 207-20. PMID 11873098.
- ↑ Chen ZM, Wang HL (October 2004). "Alteration of cytokeratin 7 and cytokeratin 20 expression profile is uniquely associated with tumorigenesis of primary adenocarcinoma of the small intestine". Am. J. Surg. Pathol. 28 (10): 1352–9. PMID 15371952.
- ↑ Dilauro, S.; Crum-Cianflone, NF. (Aug 2010). "Ileitis: when it is not Crohn's disease.". Curr Gastroenterol Rep 12 (4): 249-58. doi:10.1007/s11894-010-0112-5. PMID 20532706.
- ↑ Levy AD, Quiles AM, Miettinen M, Sobin LH (March 2005). "Gastrointestinal schwannomas: CT features with clinicopathologic correlation". AJR Am J Roentgenol 184 (3): 797–802. PMID 15728600. http://www.ajronline.org/cgi/content/full/184/3/797.
- ↑ Yamaue H, Tanimura H, Ishimoto K, Morikawa Y, Kakudo K (1996). "Nodular lymphoid hyperplasia of the terminal ileum: report of a case and the findings of an immunological analysis". Surg. Today 26 (6): 431-4. PMID 8782302.
- ↑ Ruskoné-Fourmestraux, A.; Audouin, J. (Feb 2010). "Primary gastrointestinal tract mantle cell lymphoma as multiple lymphomatous polyposis.". Best Pract Res Clin Gastroenterol 24 (1): 35-42. doi:10.1016/j.bpg.2009.12.001. PMID 20206107.
- ↑ URL: http://www.pathmax.com/gilymph.html. Accessed on: 1 April 2012.
- ↑ 11.0 11.1 McCune KH, Allen D, Cranley B (October 1992). "Small bowel diaphragm disease--strictures associated with non-steroidal anti-inflammatory drugs". Ulster Med J 61 (2): 182–4. PMC 2448949. PMID 1481311. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2448949/.
- ↑ Chung, SH.; Jo, Y.; Ryu, SR.; Ahn, SB.; Son, BK.; Kim, SH.; Park, YS.; Hong, YO. (Jun 2011). "Diaphragm disease compared with cryptogenic multifocal ulcerous stenosing enteritis.". World J Gastroenterol 17 (23): 2873-6. doi:10.3748/wjg.v17.i23.2873. PMID 21734797.



