Difference between revisions of "Glioblastoma"
Jump to navigation
Jump to search
(split out) |
Jensflorian (talk | contribs) (→IHC: moved from neuropathology tumours) |
||
| (29 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
'''Glioblastoma''' a very common malignant [[brain tumour]] in adults. | {{ Infobox diagnosis | ||
| Name = {{PAGENAME}} | |||
| Image = Glioblastoma_-_high_mag.jpg | |||
| Width = | |||
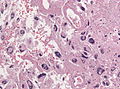
| Caption = Glioblastoma. [[H&E stain]]. | |||
| Micro = astrocytic differentiation, nuclear atypia, [[necrosis]], microvascular proliferation, +/-pseudopalisading necrosis | |||
| Subtypes = [[gliosarcoma]] | |||
| LMDDx = [[anaplastic astrocytoma]] | |||
| Stains = | |||
| IHC = GFAP +ve, IDH-1 -ve/+ve | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = brain, spinal cord | |||
| Assdx = | |||
| Syndromes = | |||
| Clinicalhx = | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = | |||
| Bloodwork = | |||
| Rads = intra-axial | |||
| Endoscopy = | |||
| Prognosis = very poor | |||
| Other = | |||
| ClinDDx = [[Metastatic_brain_tumours|metastatic brain tumours]] | |||
}} | |||
'''Glioblastoma''' a very common malignant primary [[brain tumour]] in adults. It has a very poor prognosis. | |||
It was previously known as ''glioblastoma multiforme'', abbreviated ''GBM''. | It was previously known as ''glioblastoma multiforme'', abbreviated ''GBM''. | ||
| Line 5: | Line 34: | ||
*Median survival is measured in months.<ref>{{Cite journal | last1 = Jubelirer | first1 = SJ. | title = A review of the treatment and survival rates of 138 patients with glioblastoma multiforme. | journal = W V Med J | volume = 92 | issue = 4 | pages = 186-90 | month = | year = | doi = | PMID = 8772403 }}</ref> | *Median survival is measured in months.<ref>{{Cite journal | last1 = Jubelirer | first1 = SJ. | title = A review of the treatment and survival rates of 138 patients with glioblastoma multiforme. | journal = W V Med J | volume = 92 | issue = 4 | pages = 186-90 | month = | year = | doi = | PMID = 8772403 }}</ref> | ||
*Only about 5% can expect to survive more than three years.<ref name=pmid17785346>{{Cite journal | last1 = Krex | first1 = D. | last2 = Klink | first2 = B. | last3 = Hartmann | first3 = C. | last4 = von Deimling | first4 = A. | last5 = Pietsch | first5 = T. | last6 = Simon | first6 = M. | last7 = Sabel | first7 = M. | last8 = Steinbach | first8 = JP. | last9 = Heese | first9 = O. | title = Long-term survival with glioblastoma multiforme. | journal = Brain | volume = 130 | issue = Pt 10 | pages = 2596-606 | month = Oct | year = 2007 | doi = 10.1093/brain/awm204 | PMID = 17785346 }}</ref> | *Only about 5% can expect to survive more than three years.<ref name=pmid17785346>{{Cite journal | last1 = Krex | first1 = D. | last2 = Klink | first2 = B. | last3 = Hartmann | first3 = C. | last4 = von Deimling | first4 = A. | last5 = Pietsch | first5 = T. | last6 = Simon | first6 = M. | last7 = Sabel | first7 = M. | last8 = Steinbach | first8 = JP. | last9 = Heese | first9 = O. | title = Long-term survival with glioblastoma multiforme. | journal = Brain | volume = 130 | issue = Pt 10 | pages = 2596-606 | month = Oct | year = 2007 | doi = 10.1093/brain/awm204 | PMID = 17785346 }}</ref> | ||
*Current classification recognizes three types: | |||
** Glioblastoma, IDH-wildtype (aka primary GBM, ICD-O: 9440/3). | |||
** Glioblastoma, IDH-mutant (aka secondary GBM, ICD-O: 9445/3). | |||
** Glioblastoma, NOS (lack of molecular data). | |||
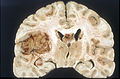
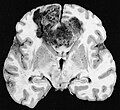
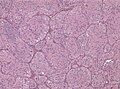
==Macroscopy== | |||
Features: | |||
* Usu. in white matter. | |||
** central necrotic core. | |||
** ill-defined borders. | |||
** yellowish to dark-brown changes. | |||
** midline shift due to tumor mass. | |||
* In the corpus callosum as bihemispheric "butterfly glioma" | |||
<gallery> | |||
File:Glioblastoma multiforme - MRT T1KM ax.jpg | Ring-enhancement in GBM (WC/Hellerhoff) | |||
File:Glioblastoma macro.jpg | Left insular GBM macroscopy (WC/Sbrandner) | |||
File:Glioblastoma multiforme.jpg | "Butterfly glioma" (WC/AFIP) | |||
</gallery> | |||
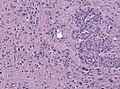
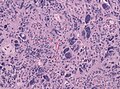
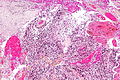
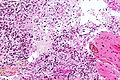
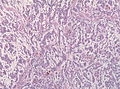
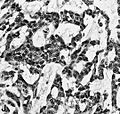
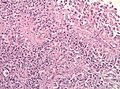
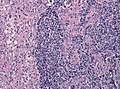
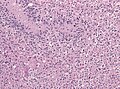
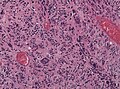
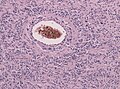
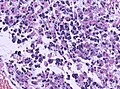
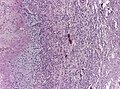
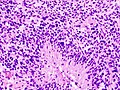
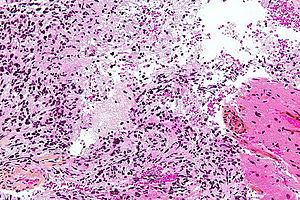
==Microscopic== | ==Microscopic== | ||
| Line 11: | Line 58: | ||
**Nuclear atypia. | **Nuclear atypia. | ||
**Necrosis. | **Necrosis. | ||
**Endothelial proliferation (AKA microvascular proliferation). | **Endothelial proliferation ([[AKA]] microvascular proliferation). | ||
**+/-"Pseudopalisading necrosis" - tumour cells lined-up like a picket fence around necrotic areas. | **+/-"Pseudopalisading necrosis" - tumour cells lined-up like a picket fence around necrotic areas. | ||
Glioblastoma variants: | |||
*Giant cell glioblastoma (ICD-O: 9441/3) | |||
** Bizarre multinucleated giant cells. | |||
** Reticulin may be abundant. | |||
** Mean age 44 years, outcome somewhat better than conventional GBM. | |||
** IDH-wildtype, but frequent p53 mutations. | |||
*Epitheloid glioblastoma (ICD-O: 9440/3) <ref>te journal | last1 = Kleinschmidt-DeMasters | first1 = BK. | last2 = Aisner | first2 = DL. | last3 = Birks | first3 = DK. | last4 = Foreman | first4 = NK. | title = Epithelioid GBMs show a high percentage of BRAF V600E mutation. | journal = Am J Surg Pathol | volume = 37 | issue = 5 | pages = 685-98 | month = May | year = 2013 | doi = 10.1097/PAS.0b013e31827f9c5e | PMID = 23552385 }}</ref> | |||
** Closely packed epithelioid to rhabdoid cells, often dicohesive. | |||
** Xanthomaous changes less common than in PXA. | |||
** Children and young adults, outcome particularly poor. | |||
** Up to 50% BRAF V600E mutations. | |||
*[[Gliosarcoma]] (ICD-O: 9442/3) | |||
Morphological patterns in Glioblastoma: | |||
* Lipidized (foamy)cells <ref>{{Cite journal | last1 = Kepes | first1 = JJ. | last2 = Rubinstein | first2 = LJ. | title = Malignant gliomas with heavily lipidized (foamy) tumor cells: a report of three cases with immunoperoxidase study. | journal = Cancer | volume = 47 | issue = 10 | pages = 2451-9 | month = May | year = 1981 | doi = | PMID = 7023643 }}</ref> | |||
* Adipocyte-like maturation <ref>{{Cite journal | last1 = Rickert | first1 = CH. | last2 = Riemenschneider | first2 = MJ. | last3 = Schachenmayr | first3 = W. | last4 = Richter | first4 = HP. | last5 = Bockhorn | first5 = J. | last6 = Reifenberger | first6 = G. | last7 = Paulus | first7 = W. | title = Glioblastoma with adipocyte-like tumor cell differentiation--histological and molecular features of a rare differentiation pattern. | journal = Brain Pathol | volume = 19 | issue = 3 | pages = 431-8 | month = Jul | year = 2009 | doi = 10.1111/j.1750-3639.2008.00199.x | PMID = 18691268 }}</ref> | |||
* Rhabdoid glioblastoma (focal loss of [[INI-1]]) <ref>{{Cite journal | last1 = Hiroyuki | first1 = M. | last2 = Ogino | first2 = J. | last3 = Takahashi | first3 = A. | last4 = Hasegawa | first4 = T. | last5 = Wakabayashi | first5 = T. | title = Rhabdoid glioblastoma: an aggressive variaty of astrocytic tumor. | journal = Nagoya J Med Sci | volume = 77 | issue = 1-2 | pages = 321-8 | month = Feb | year = 2015 | doi = | PMID = 25797998 }}</ref> | |||
* Melanotic glioblastoma <ref>{{Cite journal | last1 = Jaiswal | first1 = S. | last2 = Agrawal | first2 = V. | last3 = Vij | first3 = M. | last4 = Sahu | first4 = RN. | last5 = Jaiswal | first5 = AK. | last6 = Behari | first6 = S. | title = Glioblastoma with melanotic differentiation. | journal = Clin Neuropathol | volume = 29 | issue = 5 | pages = 330-3 | month = | year = | doi = | PMID = 20860897 }}</ref> | |||
* Glioblastoma with oligodendroglial component (no improved survival) <ref>{{Cite journal | last1 = Hegi | first1 = ME. | last2 = Janzer | first2 = RC. | last3 = Lambiv | first3 = WL. | last4 = Gorlia | first4 = T. | last5 = Kouwenhoven | first5 = MC. | last6 = Hartmann | first6 = C. | last7 = von Deimling | first7 = A. | last8 = Martinet | first8 = D. | last9 = Besuchet Schmutz | first9 = N. | title = Presence of an oligodendroglioma-like component in newly diagnosed glioblastoma identifies a pathogenetically heterogeneous subgroup and lacks prognostic value: central pathology review of the EORTC_26981/NCIC_CE.3 trial. | journal = Acta Neuropathol | volume = 123 | issue = 6 | pages = 841-52 | month = Jun | year = 2012 | doi = 10.1007/s00401-011-0938-4 | PMID = 22249618 }}</ref> | |||
*Granular cell Glioblastoma <ref>{{Cite journal | last1 = Schittenhelm | first1 = J. | last2 = Psaras | first2 = T. | title = Glioblastoma with granular cell astrocytoma features: a case report and literature review. | journal = Clin Neuropathol | volume = 29 | issue = 5 | pages = 323-9 | month = | year = | doi = | PMID = 20860896 }}</ref> | |||
*Glioblastoma with primitive neuronal component.<ref>{{Cite journal | last1 = Louis | first1 = DN. | last2 = Perry | first2 = A. | last3 = Reifenberger | first3 = G. | last4 = von Deimling | first4 = A. | last5 = Figarella-Branger | first5 = D. | last6 = Cavenee | first6 = WK. | last7 = Ohgaki | first7 = H. | last8 = Wiestler | first8 = OD. | last9 = Kleihues | first9 = P. | title = The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. | journal = Acta Neuropathol | volume = 131 | issue = 6 | pages = 803-20 | month = Jun | year = 2016 | doi = 10.1007/s00401-016-1545-1 | PMID = 27157931 }}</ref> | |||
**formerly known as: PNET-like component. | |||
**have a tendency to CSF dissemination.<ref>{{Cite journal | last1 = Perry | first1 = A. | last2 = Miller | first2 = CR. | last3 = Gujrati | first3 = M. | last4 = Scheithauer | first4 = BW. | last5 = Zambrano | first5 = SC. | last6 = Jost | first6 = SC. | last7 = Raghavan | first7 = R. | last8 = Qian | first8 = J. | last9 = Cochran | first9 = EJ. | title = Malignant gliomas with primitive neuroectodermal tumor-like components: a clinicopathologic and genetic study of 53 cases. | journal = Brain Pathol | volume = 19 | issue = 1 | pages = 81-90 | month = Jan | year = 2009 | doi = 10.1111/j.1750-3639.2008.00167.x | PMID = 18452568 }}</ref> | |||
*Small cell glioblastoma. | |||
*Ependymal-like growth patterns. | |||
*Glioneuronal tumor with neuropil-like islands.<ref>{{Cite journal | last1 = Ishizawa | first1 = K. | last2 = Hirose | first2 = T. | last3 = Sugiyama | first3 = K. | last4 = Kageji | first4 = T. | last5 = Nobusawa | first5 = S. | last6 = Homma | first6 = T. | last7 = Komori | first7 = T. | last8 = Sasaki | first8 = A. | title = Pathologic diversity of glioneuronal tumor with neuropil-like islands: a histological and immunohistochemical study with a special reference to isocitrate dehydrogenase 1 (IDH1) in 5 cases. | journal = Clin Neuropathol | volume = 31 | issue = 2 | pages = 67-76 | month = | year = | doi = | PMID = 22385787 }}</ref> | |||
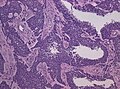
===Images=== | ===Images=== | ||
<gallery> | <gallery> | ||
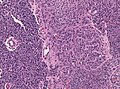
File:Gbm all in one.jpg | Core features of GBM: Necrosis, MVP and mitoses (WC/jensflorian) | |||
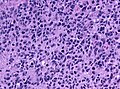
File:Glioblastoma anaplastic cells HE.jpg | Anaplastic cells in GBM (WC/jensflorian) | |||
File:Glioblastoma endothelial proliferations.jpg | Endothelial proliferations in GBM (WC/jensflorian) | |||
File:Glioblastoma mitotic activity.jpg | Mitotic activity in GBM (WC/jensflorian) | |||
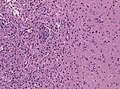
File:GBM pseudopalisading necrosis.jpg | Pseudopalisading necrosis in GBM (WC/jensflorian) | |||
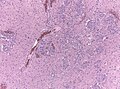
File:Glioblastoma brain infiltration zone.jpg | Diffuse brain infiltration in GBM (WC/jensflorian) | |||
File:Glioma vessels.jpg | MVP adjacent to tumor infiltration border in GBM (WC/jensflorian) | |||
Image:Glioblastoma - low mag.jpg | GBM - low mag. (WC) | |||
Image:Glioblastoma - intermed mag.jpg | GBM juxtaposed with near normal white matter - intermed. mag. (WC) | |||
Image:Glioblastoma - high mag.jpg | GBM juxtaposed with near normal white matter - high mag. (WC) | |||
Image:Glioblastoma - very high mag.jpg | GBM - very high mag. (WC) | |||
Image:Glioblastoma with extreme nuclear enlargement - high mag.jpg | GBM - high mag. (WC) | |||
Image:Glioblastoma_with_extreme_nuclear_enlargement_-_very_high_mag.jpg | Extreme nuclear enlargement in a GBM - very high mag. (WC) | Image:Glioblastoma_with_extreme_nuclear_enlargement_-_very_high_mag.jpg | Extreme nuclear enlargement in a GBM - very high mag. (WC) | ||
Image:Glioblastoma_-_high_mag.jpg | | File:Giant cell glioblastoma HE X200.jpg | Giant cell glioblastoma (WC/jensflorian) | ||
File:Adenoid glioblastoma HE.jpg | Adenoid growth pattern in GBM (WC/jensflorian) | |||
File:AFIP-00405573-Glioblastoma-Micro.jpg | Adenoid growth pattern in GBM (AFIP) | |||
File:Epitheloid glioblastoma HE.jpg | Epitheloid glioblastoma (WC/jensflorian) | |||
File:GBM PNET HE x10.jpg | GBM with PNET component (WC/jensflorian) | |||
File:Glioblastoma PNET component.jpg | GBM with PNET component (WC/jensflorian) | |||
File:Glioblastoma oligodendroglial features.jpg | GBM with oligodendroglial component (WC/jensflorian) | |||
File:Glioblastoma pleomoprhism HE.jpg | Nuclear pleomorphism in with oligodendroglial component (WC/jensflorian) | |||
File:Glioblastoma granular cell astrocytoma component.jpg | GBM with granular cell component (WC/jensflorian) | |||
File:Glioblastoma ependymal features.jpg | Glioblastoma with ependymal-like growth pattern (WC/jensflorian) | |||
File:GBM_with_Neuropil_island_HE.jpg | GBM with neuropil-like islands (WC/jensflorian) | |||
File:AFIP00405522M-GLIOBLASTOMA ARISING IN ASTROCYTOMA.jpg | Spinal cord GBM (AFIP) | |||
File:GBM mimicking melanoma.jpg | Glioblastoma mimicking a (amelanotic) melanoma (WC/jensflorian) | |||
File:GBM layers.jpg | Resection borders in a recurrent GBM (WC/jensflorian) | |||
File:Glioblastoma-radiation_changes_HE.jpg | Radiation changes in a recurrent GBM (WC/jensflorian) | |||
File:GBM_nested_epithelial.jpg | Nested epitheloid appearance in a GBM specimen (WC/jensflorian) | |||
Image:Glioblastoma_%281%29.jpg | Glioblastoma - pseudopalisading of tumour cells (WC) | |||
Image:Glioblastoma_-_high_mag.jpg | Glioblastoma with fragment of near-normal white matter - high mag. (WC) | |||
Image:Anaplastic_astrocytoma_-_very_high_mag_-_cropped.jpg | Anaplastic astrocytoma - very high mag. (WC) | |||
</gallery> | </gallery> | ||
www: | |||
*[http://moon.ouhsc.edu/kfung/jty1/OPAQ/PathQuiz/PQ-Images/N0A002-1.gif Microvascular proliferation in a GBM (ouhsc.edu)]. | |||
*[http://cancerres.aacrjournals.org/content/64/3/920/F7.expansion.html Pseudopalisading necrosis in GBM (aacrjournals.org)]. | |||
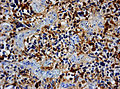
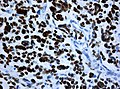
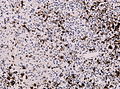
==IHC== | |||
*GFAP +ve (cytoplasm). | *GFAP +ve (cytoplasm). | ||
*IDH-1 -ve. | *[[MAP2]] +ve. | ||
**+ve if developed from lower grade astrocytoma. ( | *[[IDH-1]] -ve (95%). | ||
**+ve if developed from lower grade astrocytoma (secondary GBM) -> classify tumor as Glioblastoma, IDH-mutant. | |||
*[[WT-1]] +ve (cytoplasm). | |||
*p53 +ve (70%). | |||
*Neurofilament -ve. | |||
*Synaptophysin -ve (residual Cortex may be +ve). | |||
*panCK -ve (except for GBM with epithelial component). | |||
*[[ATRX]]: +ve (no loss, nuclei) | |||
**-ve if developed from lower grade astrocytoma (secondary GBM). | |||
*EMA: Dot-like expression less common than in [[ependymoma]]s. | |||
*MIB-1 usu. 15-30%, but varies greatly. | |||
<gallery> | |||
File:Glioblastoma GFAP.jpg | GFAP immunostaining in GBM (WC/Marvin 101) | |||
File:Wilms tumor protein wt1 immunohistocehmistry glioblastoma.JPG | WT1 immunostaining in GBM (WC/jensflorian) | |||
File:Glioblastoma P53.jpg | GBM with strong p53 immunreactivity (WC/jensflorian) | |||
File:Glioblastoma Ck7.jpg|CK7 staining in glioblastoma with epithelial component (WC/jensflorian) | |||
File:GBM_with_Neuropil_island_MIB1.jpg|Reduced proliferation in neuropil-like islands (MIB1). | |||
File:GBM_with_Neuropil_island_Syn.jpg |Synaptophysin immunoreactivity in neuropil-like islands (WC/jensflorian). | |||
Image:Anaplastic_astrocytoma_-_gfap_-_very_high_mag.jpg | Anaplastic astrocytic tumor cells - GFAP - very high mag. (WC) | |||
</gallery> | |||
==Molecular== | |||
*IDH1/2 sequencing in cases below 55 years is mandatory to separate between Glioblastoma, IDH-wildtype and Glioblastoma IDH-mutant. | |||
** In cases above 55 years, negative IDH1 R132H immunohistochemistry may be sufficient. | |||
* 70% of IDH-wildtype glioblastoma show chr.7 gain and chr.10 loss.<ref>{{Cite journal | last1 = Ceccarelli | first1 = M. | last2 = Barthel | first2 = FP. | last3 = Malta | first3 = TM. | last4 = Sabedot | first4 = TS. | last5 = Salama | first5 = SR. | last6 = Murray | first6 = BA. | last7 = Morozova | first7 = O. | last8 = Newton | first8 = Y. | last9 = Radenbaugh | first9 = A. | title = Molecular Profiling Reveals Biologically Discrete Subsets and Pathways of Progression in Diffuse Glioma. | journal = Cell | volume = 164 | issue = 3 | pages = 550-63 | month = Jan | year = 2016 | doi = 10.1016/j.cell.2015.12.028 | PMID = 26824661 }}</ref> | |||
*Seen in inherited tumor syndromes: | |||
**[[Lynch syndrome]] | |||
**[[Neurofibromatosis 1]] | |||
**[[Li-Fraumeni syndrome]] | |||
**Turcot-Syndrome | |||
*Most common alterations (TCGA<ref>{{Cite journal | last1 = Verhaak | first1 = RG. | last2 = Hoadley | first2 = KA. | last3 = Purdom | first3 = E. | last4 = Wang | first4 = V. | last5 = Qi | first5 = Y. | last6 = Wilkerson | first6 = MD. | last7 = Miller | first7 = CR. | last8 = Ding | first8 = L. | last9 = Golub | first9 = T. | title = Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. | journal = Cancer Cell | volume = 17 | issue = 1 | pages = 98-110 | month = Jan | year = 2010 | doi = 10.1016/j.ccr.2009.12.020 | PMID = 20129251 }}</ref>) | |||
**Tp53 (42% of the tumors mutated) | |||
**PTEN (33%). | |||
**NF1 (21%). | |||
**EGFR (18%). | |||
**RB1 (11%). | |||
**PI3K-pathway genes (7-10%). | |||
*Pediatric glioblastoma | |||
**are morphologically indistinct from adult GBM. | |||
**show frequent H3F3A mutations and PDGFRA mutations (Note: H3F3A K27M mutations are classified as [[Astrocytoma#H3.3_K27M_mutated_glioma_of_the_midline|K27 mutated midline glioma]]). | |||
**Consider Epithelioid GBM, when BRAF V600E mutated. | |||
*Diagnostic/therapeutic relevant markers: | |||
**[[MGMT]] promoter methylation status<ref>{{Cite journal | last1 = Quillien | first1 = V. | last2 = Lavenu | first2 = A. | last3 = Karayan-Tapon | first3 = L. | last4 = Carpentier | first4 = C. | last5 = Labussière | first5 = M. | last6 = Lesimple | first6 = T. | last7 = Chinot | first7 = O. | last8 = Wager | first8 = M. | last9 = Honnorat | first9 = J. | title = Comparative assessment of 5 methods (methylation-specific polymerase chain reaction, MethyLight, pyrosequencing, methylation-sensitive high-resolution melting, and immunohistochemistry) to analyze O6-methylguanine-DNA-methyltranferase in a series of 100 glioblastoma patients. | journal = Cancer | volume = 118 | issue = 17 | pages = 4201-11 | month = Sep | year = 2012 | doi = 10.1002/cncr.27392 | PMID = 22294349 }}</ref> | |||
**Absence of LOH 1p/19q (otherwise classify tumor as [[oligodendroglioma]]).<ref>{{Cite journal | last1 = Masui | first1 = K. | last2 = Mischel | first2 = PS. | last3 = Reifenberger | first3 = G. | title = Molecular classification of gliomas. | journal = Handb Clin Neurol | volume = 134 | issue = | pages = 97-120 | month = | year = 2016 | doi = 10.1016/B978-0-12-802997-8.00006-2 | PMID = 26948350 }}</ref> | |||
==See also== | ==See also== | ||
Latest revision as of 09:07, 14 April 2022
| Glioblastoma | |
|---|---|
| Diagnosis in short | |
 Glioblastoma. H&E stain. | |
|
| |
| LM | astrocytic differentiation, nuclear atypia, necrosis, microvascular proliferation, +/-pseudopalisading necrosis |
| Subtypes | gliosarcoma |
| LM DDx | anaplastic astrocytoma |
| IHC | GFAP +ve, IDH-1 -ve/+ve |
| Site | brain, spinal cord |
|
| |
| Radiology | intra-axial |
| Prognosis | very poor |
| Clin. DDx | metastatic brain tumours |
Glioblastoma a very common malignant primary brain tumour in adults. It has a very poor prognosis.
It was previously known as glioblastoma multiforme, abbreviated GBM.
General
- Median survival is measured in months.[1]
- Only about 5% can expect to survive more than three years.[2]
- Current classification recognizes three types:
- Glioblastoma, IDH-wildtype (aka primary GBM, ICD-O: 9440/3).
- Glioblastoma, IDH-mutant (aka secondary GBM, ICD-O: 9445/3).
- Glioblastoma, NOS (lack of molecular data).
Macroscopy
Features:
- Usu. in white matter.
- central necrotic core.
- ill-defined borders.
- yellowish to dark-brown changes.
- midline shift due to tumor mass.
- In the corpus callosum as bihemispheric "butterfly glioma"
Microscopic
Features:
- Astrocytic tumour with:
- Nuclear atypia.
- Necrosis.
- Endothelial proliferation (AKA microvascular proliferation).
- +/-"Pseudopalisading necrosis" - tumour cells lined-up like a picket fence around necrotic areas.
Glioblastoma variants:
- Giant cell glioblastoma (ICD-O: 9441/3)
- Bizarre multinucleated giant cells.
- Reticulin may be abundant.
- Mean age 44 years, outcome somewhat better than conventional GBM.
- IDH-wildtype, but frequent p53 mutations.
- Epitheloid glioblastoma (ICD-O: 9440/3) [3]
- Closely packed epithelioid to rhabdoid cells, often dicohesive.
- Xanthomaous changes less common than in PXA.
- Children and young adults, outcome particularly poor.
- Up to 50% BRAF V600E mutations.
- Gliosarcoma (ICD-O: 9442/3)
Morphological patterns in Glioblastoma:
- Lipidized (foamy)cells [4]
- Adipocyte-like maturation [5]
- Rhabdoid glioblastoma (focal loss of INI-1) [6]
- Melanotic glioblastoma [7]
- Glioblastoma with oligodendroglial component (no improved survival) [8]
- Granular cell Glioblastoma [9]
- Glioblastoma with primitive neuronal component.[10]
- formerly known as: PNET-like component.
- have a tendency to CSF dissemination.[11]
- Small cell glioblastoma.
- Ependymal-like growth patterns.
- Glioneuronal tumor with neuropil-like islands.[12]
Images
www:
- Microvascular proliferation in a GBM (ouhsc.edu).
- Pseudopalisading necrosis in GBM (aacrjournals.org).
IHC
- GFAP +ve (cytoplasm).
- MAP2 +ve.
- IDH-1 -ve (95%).
- +ve if developed from lower grade astrocytoma (secondary GBM) -> classify tumor as Glioblastoma, IDH-mutant.
- WT-1 +ve (cytoplasm).
- p53 +ve (70%).
- Neurofilament -ve.
- Synaptophysin -ve (residual Cortex may be +ve).
- panCK -ve (except for GBM with epithelial component).
- ATRX: +ve (no loss, nuclei)
- -ve if developed from lower grade astrocytoma (secondary GBM).
- EMA: Dot-like expression less common than in ependymomas.
- MIB-1 usu. 15-30%, but varies greatly.
Molecular
- IDH1/2 sequencing in cases below 55 years is mandatory to separate between Glioblastoma, IDH-wildtype and Glioblastoma IDH-mutant.
- In cases above 55 years, negative IDH1 R132H immunohistochemistry may be sufficient.
- 70% of IDH-wildtype glioblastoma show chr.7 gain and chr.10 loss.[13]
- Seen in inherited tumor syndromes:
- Lynch syndrome
- Neurofibromatosis 1
- Li-Fraumeni syndrome
- Turcot-Syndrome
- Most common alterations (TCGA[14])
- Tp53 (42% of the tumors mutated)
- PTEN (33%).
- NF1 (21%).
- EGFR (18%).
- RB1 (11%).
- PI3K-pathway genes (7-10%).
- Pediatric glioblastoma
- are morphologically indistinct from adult GBM.
- show frequent H3F3A mutations and PDGFRA mutations (Note: H3F3A K27M mutations are classified as K27 mutated midline glioma).
- Consider Epithelioid GBM, when BRAF V600E mutated.
- Diagnostic/therapeutic relevant markers:
- MGMT promoter methylation status[15]
- Absence of LOH 1p/19q (otherwise classify tumor as oligodendroglioma).[16]
See also
References
- ↑ Jubelirer, SJ.. "A review of the treatment and survival rates of 138 patients with glioblastoma multiforme.". W V Med J 92 (4): 186-90. PMID 8772403.
- ↑ Krex, D.; Klink, B.; Hartmann, C.; von Deimling, A.; Pietsch, T.; Simon, M.; Sabel, M.; Steinbach, JP. et al. (Oct 2007). "Long-term survival with glioblastoma multiforme.". Brain 130 (Pt 10): 2596-606. doi:10.1093/brain/awm204. PMID 17785346.
- ↑ te journal | last1 = Kleinschmidt-DeMasters | first1 = BK. | last2 = Aisner | first2 = DL. | last3 = Birks | first3 = DK. | last4 = Foreman | first4 = NK. | title = Epithelioid GBMs show a high percentage of BRAF V600E mutation. | journal = Am J Surg Pathol | volume = 37 | issue = 5 | pages = 685-98 | month = May | year = 2013 | doi = 10.1097/PAS.0b013e31827f9c5e | PMID = 23552385 }}
- ↑ Kepes, JJ.; Rubinstein, LJ. (May 1981). "Malignant gliomas with heavily lipidized (foamy) tumor cells: a report of three cases with immunoperoxidase study.". Cancer 47 (10): 2451-9. PMID 7023643.
- ↑ Rickert, CH.; Riemenschneider, MJ.; Schachenmayr, W.; Richter, HP.; Bockhorn, J.; Reifenberger, G.; Paulus, W. (Jul 2009). "Glioblastoma with adipocyte-like tumor cell differentiation--histological and molecular features of a rare differentiation pattern.". Brain Pathol 19 (3): 431-8. doi:10.1111/j.1750-3639.2008.00199.x. PMID 18691268.
- ↑ Hiroyuki, M.; Ogino, J.; Takahashi, A.; Hasegawa, T.; Wakabayashi, T. (Feb 2015). "Rhabdoid glioblastoma: an aggressive variaty of astrocytic tumor.". Nagoya J Med Sci 77 (1-2): 321-8. PMID 25797998.
- ↑ Jaiswal, S.; Agrawal, V.; Vij, M.; Sahu, RN.; Jaiswal, AK.; Behari, S.. "Glioblastoma with melanotic differentiation.". Clin Neuropathol 29 (5): 330-3. PMID 20860897.
- ↑ Hegi, ME.; Janzer, RC.; Lambiv, WL.; Gorlia, T.; Kouwenhoven, MC.; Hartmann, C.; von Deimling, A.; Martinet, D. et al. (Jun 2012). "Presence of an oligodendroglioma-like component in newly diagnosed glioblastoma identifies a pathogenetically heterogeneous subgroup and lacks prognostic value: central pathology review of the EORTC_26981/NCIC_CE.3 trial.". Acta Neuropathol 123 (6): 841-52. doi:10.1007/s00401-011-0938-4. PMID 22249618.
- ↑ Schittenhelm, J.; Psaras, T.. "Glioblastoma with granular cell astrocytoma features: a case report and literature review.". Clin Neuropathol 29 (5): 323-9. PMID 20860896.
- ↑ Louis, DN.; Perry, A.; Reifenberger, G.; von Deimling, A.; Figarella-Branger, D.; Cavenee, WK.; Ohgaki, H.; Wiestler, OD. et al. (Jun 2016). "The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary.". Acta Neuropathol 131 (6): 803-20. doi:10.1007/s00401-016-1545-1. PMID 27157931.
- ↑ Perry, A.; Miller, CR.; Gujrati, M.; Scheithauer, BW.; Zambrano, SC.; Jost, SC.; Raghavan, R.; Qian, J. et al. (Jan 2009). "Malignant gliomas with primitive neuroectodermal tumor-like components: a clinicopathologic and genetic study of 53 cases.". Brain Pathol 19 (1): 81-90. doi:10.1111/j.1750-3639.2008.00167.x. PMID 18452568.
- ↑ Ishizawa, K.; Hirose, T.; Sugiyama, K.; Kageji, T.; Nobusawa, S.; Homma, T.; Komori, T.; Sasaki, A.. "Pathologic diversity of glioneuronal tumor with neuropil-like islands: a histological and immunohistochemical study with a special reference to isocitrate dehydrogenase 1 (IDH1) in 5 cases.". Clin Neuropathol 31 (2): 67-76. PMID 22385787.
- ↑ Ceccarelli, M.; Barthel, FP.; Malta, TM.; Sabedot, TS.; Salama, SR.; Murray, BA.; Morozova, O.; Newton, Y. et al. (Jan 2016). "Molecular Profiling Reveals Biologically Discrete Subsets and Pathways of Progression in Diffuse Glioma.". Cell 164 (3): 550-63. doi:10.1016/j.cell.2015.12.028. PMID 26824661.
- ↑ Verhaak, RG.; Hoadley, KA.; Purdom, E.; Wang, V.; Qi, Y.; Wilkerson, MD.; Miller, CR.; Ding, L. et al. (Jan 2010). "Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1.". Cancer Cell 17 (1): 98-110. doi:10.1016/j.ccr.2009.12.020. PMID 20129251.
- ↑ Quillien, V.; Lavenu, A.; Karayan-Tapon, L.; Carpentier, C.; Labussière, M.; Lesimple, T.; Chinot, O.; Wager, M. et al. (Sep 2012). "Comparative assessment of 5 methods (methylation-specific polymerase chain reaction, MethyLight, pyrosequencing, methylation-sensitive high-resolution melting, and immunohistochemistry) to analyze O6-methylguanine-DNA-methyltranferase in a series of 100 glioblastoma patients.". Cancer 118 (17): 4201-11. doi:10.1002/cncr.27392. PMID 22294349.
- ↑ Masui, K.; Mischel, PS.; Reifenberger, G. (2016). "Molecular classification of gliomas.". Handb Clin Neurol 134: 97-120. doi:10.1016/B978-0-12-802997-8.00006-2. PMID 26948350.