Difference between revisions of "Classic vulvar intraepithelial neoplasia"
(split out) |
|||
| (8 intermediate revisions by the same user not shown) | |||
| Line 1: | Line 1: | ||
{{ Infobox diagnosis | |||
| Name = {{PAGENAME}} | |||
| Image = Vulvar_intraepithelial_neoplasia3_1.jpg | |||
| Width = | |||
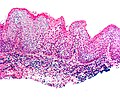
| Caption = Classic vulvar intraepithelial neoplasia. [[H&E stain]]. | |||
| Synonyms = usual vulvar intraepithelial neoplasia | |||
| Micro = increased [[NC ratio]], multinucleation, lack of maturation to surface (not very useful -- unlike in the cervix), +/-non-basal mitoses, +/-atypical mitoses | |||
| Subtypes = | |||
| LMDDx = [[vulvar squamous cell carcinoma]], [[condyloma acuminatum]], [[dermatomycosis]] | |||
| Stains = | |||
| IHC = p16 +ve, p53 -ve, Ki-67 - suprabasal staining | |||
| EM = | |||
| Molecular = | |||
| IF = | |||
| Gross = | |||
| Grossing = | |||
| Site = [[vulva]] | |||
| Assdx = [[vulvar squamous cell carcinoma]], other [[HPV]] lesions | |||
| Syndromes = | |||
| Clinicalhx = young women | |||
| Signs = | |||
| Symptoms = | |||
| Prevalence = uncommon | |||
| Bloodwork = | |||
| Rads = | |||
| Endoscopy = | |||
| Prognosis = | |||
| Other = | |||
| ClinDDx = | |||
| Tx = | |||
}} | |||
'''Classic vulvar intraepithelial neoplasia''', abbreviated '''classic VIN''', is a pre-neoplastic lesion of the [[vulva]] strongly associated with the [[human papilloma virus]]. | |||
It | It is also known as '''usual vulvar intraepithelial neoplasia''', abbreviated '''uVIN'''.<ref name=pmid24399036>{{Cite journal | last1 = Reyes | first1 = MC. | last2 = Cooper | first2 = K. | title = An update on vulvar intraepithelial neoplasia: terminology and a practical approach to diagnosis. | journal = J Clin Pathol | volume = | issue = | pages = | month = Jan | year = 2014 | doi = 10.1136/jclinpath-2013-202117 | PMID = 24399036 }}</ref> Despite being called "usual", it is less common than the other form of [[vulvar intraepithelial neoplasia]] ([[differentiated vulvar intraepithelial neoplasia]]). | ||
==General== | ==General== | ||
| Line 27: | Line 58: | ||
DDx: | DDx: | ||
*[[Condyloma acuminatum]]. | *[[Condyloma acuminatum]]. | ||
*[[Vulvar squamous cell carcinoma]]. | *[[Vulvar squamous cell carcinoma]], esp. warty type. | ||
*[[Extramammary Paget disease]]. | *[[Extramammary Paget disease]]. | ||
*[[Dermatomycosis]] (fungal infection) - esp. [[candidiasis]]. | *[[Dermatomycosis]] (fungal infection) - esp. [[candidiasis]]. | ||
===Images=== | ===Images=== | ||
<gallery> | |||
Image:Vulvar_intraepithelial_neoplasia3_1.jpg | VIN III. (WC) | |||
Image:Vulvar_intraepithelial_neoplasia3_2.jpg | VIN III. (WC) | |||
</gallery> | |||
*[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3150314/figure/F3/ VIN I - koilocytes (nih.gov)].<ref name=pmid21702970/> | *[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3150314/figure/F3/ VIN I - koilocytes (nih.gov)].<ref name=pmid21702970/> | ||
*[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3150314/figure/F4/ VIN I (nih.gov)].<ref name=pmid21702970>{{Cite journal | last1 = Kotsopoulos | first1 = IC. | last2 = Tampakoudis | first2 = GP. | last3 = Evaggelinos | first3 = DG. | last4 = Nikolaidou | first4 = AI. | last5 = Fytili | first5 = PA. | last6 = Kartsiounis | first6 = VC. | last7 = Gerasimidou | first7 = DK. | title = Implication of human papillomavirus-66 in vulvar carcinoma: a case report. | journal = J Med Case Rep | volume = 5 | issue = | pages = 232 | month = | year = 2011 | doi = 10.1186/1752-1947-5-232 | PMID = 21702970 | PMC = 3150314 }}</ref> | *[http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3150314/figure/F4/ VIN I (nih.gov)].<ref name=pmid21702970>{{Cite journal | last1 = Kotsopoulos | first1 = IC. | last2 = Tampakoudis | first2 = GP. | last3 = Evaggelinos | first3 = DG. | last4 = Nikolaidou | first4 = AI. | last5 = Fytili | first5 = PA. | last6 = Kartsiounis | first6 = VC. | last7 = Gerasimidou | first7 = DK. | title = Implication of human papillomavirus-66 in vulvar carcinoma: a case report. | journal = J Med Case Rep | volume = 5 | issue = | pages = 232 | month = | year = 2011 | doi = 10.1186/1752-1947-5-232 | PMID = 21702970 | PMC = 3150314 }}</ref> | ||
*[http://www.flickr.com/photos/euthman/2658773592/ VIN III (flickr.com)]. | *[http://www.flickr.com/photos/euthman/2658773592/ VIN III (flickr.com)]. | ||
*[http://www.brown.edu/Courses/Digital_Path/systemic_path/female/warty_VIN.html VIN (brown.edu)]. | *[http://www.brown.edu/Courses/Digital_Path/systemic_path/female/warty_VIN.html VIN (brown.edu)]. | ||
| Line 52: | Line 86: | ||
- NEGATIVE FOR INVASIVE MALIGNANCY. | - NEGATIVE FOR INVASIVE MALIGNANCY. | ||
</pre> | </pre> | ||
====VIN II==== | |||
<pre> | |||
LEFT LABIUM MINUS, PUNCH BIOPSY: | |||
- CLASSIC VULVAR INTRAEPITHELIAL NEOPLASIA (cVIN) II (MODERATE DYSPLASIA). | |||
- LICHEN SCLEROSUS. | |||
COMMENT: | |||
Immunostains: | |||
POSITIVE: p16 (strong, diffuse - lower 2/3 of the epithelium). | |||
NEGATIVE: HMB-45, S-100, p53 (weak, patchy, superficial squamous cells). | |||
PROLIFERATION (Ki-67): increased, marks superficial squamous cells (compatible with | |||
high-grade lesion). | |||
</pre> | |||
=====Micro===== | |||
The sections show a punch biopsy of skin. Compact hyperkeratosis and hypergranulosis is | |||
present. The epidermis is edematous, has moderately atypical cells in the lower two thirds | |||
of the epithelium and mitotic activity. Several suprabasal mitoses are present. Apoptotic | |||
keratinocytes are present. Granular yellow pigment (hemosiderin?) is present in the | |||
epidermis. The epidermis is not significantly thickened. The lesional cells extend | |||
to the lateral edges of the tissue. | |||
====VIN III==== | ====VIN III==== | ||
| Line 61: | Line 117: | ||
- NEGATIVE FOR INVASIVE MALIGNANCY. | - NEGATIVE FOR INVASIVE MALIGNANCY. | ||
</pre> | </pre> | ||
==See also== | ==See also== | ||
*[[Vulva]]. | *[[Vulva]]. | ||
*[[Differentiated vulvar intraepithelial neoplasia]]. | |||
==References== | ==References== | ||
Latest revision as of 18:35, 27 February 2014
| Classic vulvar intraepithelial neoplasia | |
|---|---|
| Diagnosis in short | |
 Classic vulvar intraepithelial neoplasia. H&E stain. | |
|
| |
| Synonyms | usual vulvar intraepithelial neoplasia |
|
| |
| LM | increased NC ratio, multinucleation, lack of maturation to surface (not very useful -- unlike in the cervix), +/-non-basal mitoses, +/-atypical mitoses |
| LM DDx | vulvar squamous cell carcinoma, condyloma acuminatum, dermatomycosis |
| IHC | p16 +ve, p53 -ve, Ki-67 - suprabasal staining |
| Site | vulva |
|
| |
| Associated Dx | vulvar squamous cell carcinoma, other HPV lesions |
| Clinical history | young women |
| Prevalence | uncommon |
Classic vulvar intraepithelial neoplasia, abbreviated classic VIN, is a pre-neoplastic lesion of the vulva strongly associated with the human papilloma virus.
It is also known as usual vulvar intraepithelial neoplasia, abbreviated uVIN.[1] Despite being called "usual", it is less common than the other form of vulvar intraepithelial neoplasia (differentiated vulvar intraepithelial neoplasia).
General
Epidemiology:
- Classic VIN, like CIN, is associated with HPV and seen in younger women.
- May be multifocal, i.e. associated with cervical (CIN) or vaginal (VAIN) lesions;[2] multifocality has a strongly association with immunosuppression.[3]
Classic VIN is graded like cervical pre-cancerous lesions:
- VIN I.
- DDx: condyloma acuminatum.[4]
- Uncommon.
- VIN II.
- Not common.
- VIN III.
- Commonly seen.
Microscopic
Features:
- Increased NC ratio.
- Multinucleation.
- Lack of maturation to surface (not very useful -- unlike in the cervix).[5]
- May have "vertical streaming" - the long axis of the cells are perpendicular to the free surface & basement membrane.
- Apical mitoses.
DDx:
- Condyloma acuminatum.
- Vulvar squamous cell carcinoma, esp. warty type.
- Extramammary Paget disease.
- Dermatomycosis (fungal infection) - esp. candidiasis.
Images
IHC
- Classic VIN: p16 +ve, p53 -ve.
- Differentiated VIN: p16 -ve, p53 +ve.[7]
Note:
- p16 can be thought of as a poor man's HPV test.
Sign out
VIN I
VULVA, BIOPSY: - CLASSIC VULVAR INTRAEPITHELIAL NEOPLASIA (VIN) I (MILD DYSPLASIA). - NEGATIVE FOR INVASIVE MALIGNANCY.
VIN II
LEFT LABIUM MINUS, PUNCH BIOPSY:
- CLASSIC VULVAR INTRAEPITHELIAL NEOPLASIA (cVIN) II (MODERATE DYSPLASIA).
- LICHEN SCLEROSUS.
COMMENT:
Immunostains:
POSITIVE: p16 (strong, diffuse - lower 2/3 of the epithelium).
NEGATIVE: HMB-45, S-100, p53 (weak, patchy, superficial squamous cells).
PROLIFERATION (Ki-67): increased, marks superficial squamous cells (compatible with
high-grade lesion).
Micro
The sections show a punch biopsy of skin. Compact hyperkeratosis and hypergranulosis is present. The epidermis is edematous, has moderately atypical cells in the lower two thirds of the epithelium and mitotic activity. Several suprabasal mitoses are present. Apoptotic keratinocytes are present. Granular yellow pigment (hemosiderin?) is present in the epidermis. The epidermis is not significantly thickened. The lesional cells extend to the lateral edges of the tissue.
VIN III
VULVA, EXCISION: - CLASSIC VULVAR INTRAEPITHELIAL NEOPLASIA (VIN) III (SEVERE DYSPLASIA) WITH FOCAL ULCERATION. - MARGIN FOCALLY POSITIVE FOR VIN III. - NEGATIVE FOR INVASIVE MALIGNANCY.
See also
References
- ↑ Reyes, MC.; Cooper, K. (Jan 2014). "An update on vulvar intraepithelial neoplasia: terminology and a practical approach to diagnosis.". J Clin Pathol. doi:10.1136/jclinpath-2013-202117. PMID 24399036.
- ↑ Pai, K.; Pai, S.; Gupta, A.; Rao, P.; Renjhen, P. (Oct 2006). "Synchronous vulvar intraepithelial neoplasia (VIN) of warty type and cervical intraepithelial neoplasia (CIN): case report.". Indian J Pathol Microbiol 49 (4): 585-7. PMID 17183865.
- ↑ Ait Menguellet, S.; Collinet, P.; Houfflin Debarge, V.; Nayama, M.; Vinatier, D.; Leroy, JL. (May 2007). "Management of multicentric lesions of the lower genital tract.". Eur J Obstet Gynecol Reprod Biol 132 (1): 116-20. doi:10.1016/j.ejogrb.2006.04.011. PMID 16713062.
- ↑ Rufforny, I.; Wilkinson, EJ.; Liu, C.; Zhu, H.; Buteral, M.; Massoll, NA. (Apr 2005). "Human papillomavirus infection and p16(INK4a) protein expression in vulvar intraepithelial neoplasia and invasive squamous cell carcinoma.". J Low Genit Tract Dis 9 (2): 108-13. PMID 15870532.
- ↑ LAE. February 2009.
- ↑ 6.0 6.1 Kotsopoulos, IC.; Tampakoudis, GP.; Evaggelinos, DG.; Nikolaidou, AI.; Fytili, PA.; Kartsiounis, VC.; Gerasimidou, DK. (2011). "Implication of human papillomavirus-66 in vulvar carcinoma: a case report.". J Med Case Rep 5: 232. doi:10.1186/1752-1947-5-232. PMC 3150314. PMID 21702970. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3150314/.
- ↑ Pinto, AP.; Miron, A.; Yassin, Y.; Monte, N.; Woo, TY.; Mehra, KK.; Medeiros, F.; Crum, CP. (Mar 2010). "Differentiated vulvar intraepithelial neoplasia contains Tp53 mutations and is genetically linked to vulvar squamous cell carcinoma.". Mod Pathol 23 (3): 404-12. doi:10.1038/modpathol.2009.179. PMID 20062014.