Difference between revisions of "Pineal gland"
Jump to navigation
Jump to search
Jensflorian (talk | contribs) (→Overview: +pineal gland cyst) |
m (vauthors -> authors) |
||
| (9 intermediate revisions by 2 users not shown) | |||
| Line 23: | Line 23: | ||
**[[Meningioma]]s. | **[[Meningioma]]s. | ||
==Pineal gland cyst== | |||
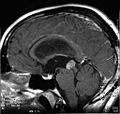
*Quite common. <ref name=pmid17885233> {{Cite journal | last1 = Pu | first1 = Y. | last2 = Mahankali | first2 = S. | last3 = Hou | first3 = J. | last4 = Li | first4 = J. | last5 = Lancaster | first5 = JL. | last6 = Gao | first6 = JH. | last7 = Appelbaum | first7 = DE. | last8 = Fox | first8 = PT. | title = High prevalence of pineal cysts in healthy adults demonstrated by high-resolution, noncontrast brain MR imaging. | journal = AJNR Am J Neuroradiol | volume = 28 | issue = 9 | pages = 1706-9 | month = Oct | year = 2007 | doi = 10.3174/ajnr.A0656 | PMID = 17885233 }}</ref> | *Quite common. <ref name=pmid17885233> {{Cite journal | last1 = Pu | first1 = Y. | last2 = Mahankali | first2 = S. | last3 = Hou | first3 = J. | last4 = Li | first4 = J. | last5 = Lancaster | first5 = JL. | last6 = Gao | first6 = JH. | last7 = Appelbaum | first7 = DE. | last8 = Fox | first8 = PT. | title = High prevalence of pineal cysts in healthy adults demonstrated by high-resolution, noncontrast brain MR imaging. | journal = AJNR Am J Neuroradiol | volume = 28 | issue = 9 | pages = 1706-9 | month = Oct | year = 2007 | doi = 10.3174/ajnr.A0656 | PMID = 17885233 }}</ref> | ||
*large cysts can cause CSF obstruction. <ref>{{Cite journal | last1 = Mena | first1 = H. | last2 = Armonda | first2 = RA. | last3 = Ribas | first3 = JL. | last4 = Ondra | first4 = SL. | last5 = Rushing | first5 = EJ. | title = Nonneoplastic pineal cysts: a clinicopathologic study of twenty-one cases. | journal = Ann Diagn Pathol | volume = 1 | issue = 1 | pages = 11-8 | month = Oct | year = 1997 | doi = | PMID = 9869821 }}</ref> | *large cysts can cause CSF obstruction. <ref>{{Cite journal | last1 = Mena | first1 = H. | last2 = Armonda | first2 = RA. | last3 = Ribas | first3 = JL. | last4 = Ondra | first4 = SL. | last5 = Rushing | first5 = EJ. | title = Nonneoplastic pineal cysts: a clinicopathologic study of twenty-one cases. | journal = Ann Diagn Pathol | volume = 1 | issue = 1 | pages = 11-8 | month = Oct | year = 1997 | doi = | PMID = 9869821 }}</ref> | ||
< | <gallery> | ||
File:Pinealiszyste.jpg | Pineal gland cyst found at autopsy. (WC/Marvin101) | File:Pinealiszyste.jpg | Pineal gland cyst found at autopsy. (WC/Marvin101) | ||
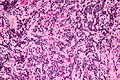
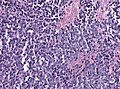
File:Pineal_gland_cyst_low_mag_HE.jpg | Pineal gland cyst. HE, low mag. (WC/jensflorian) | File:Pineal_gland_cyst_low_mag_HE.jpg | Pineal gland cyst. HE, low mag. (WC/jensflorian) | ||
| Line 33: | Line 33: | ||
</gallery> | </gallery> | ||
==Pineocytoma== | ==Pineocytoma== | ||
| Line 87: | Line 86: | ||
*Usually no pinecytomatous rosettes. | *Usually no pinecytomatous rosettes. | ||
*High pleomorphism possible. | *High pleomorphism possible. | ||
===Molecular=== | |||
* Insertions in KBTBD4.<ref name="pmid31768671">{{cite journal |authors=Pfaff E, Aichmüller C, Sill M, Stichel D, Snuderl M, Karajannis MA, Schuhmann MU, Schittenhelm J, Hasselblatt M, Thomas C, Korshunov A, Rhizova M, Wittmann A, Kaufhold A, Iskar M, Ketteler P, Lohmann D, Orr BA, Ellison DW, von Hoff K, Mynarek M, Rutkowski S, Sahm F, von Deimling A, Lichter P, Kool M, Zapatka M, Pfister SM, Jones DTW |title=Molecular subgrouping of primary pineal parenchymal tumors reveals distinct subtypes correlated with clinical parameters and genetic alterations |journal=Acta Neuropathol |volume=139 |issue=2 |pages=243–257 |date=February 2020 |pmid=31768671 |doi=10.1007/s00401-019-02101-0 |url=}}</ref> | |||
Images: | Images: | ||
| Line 96: | Line 99: | ||
</gallery> | </gallery> | ||
==Papillary | ==Papillary tumour of pineal region (PTPR)== | ||
===General=== | ===General=== | ||
*Very rare neuoepithelial tumor of adults. | *Very rare neuoepithelial tumor of adults. | ||
| Line 128: | Line 131: | ||
* EMA mostly -ve. | * EMA mostly -ve. | ||
* NF and Kir 7.1-ve. | * NF and Kir 7.1-ve. | ||
===Molecular=== | |||
* PTEN alterations. <ref name="pmid26113311">{{cite journal |authors=Heim S, Sill M, Jones DT, Vasiljevic A, Jouvet A, Fèvre-Montange M, Wesseling P, Beschorner R, Mittelbronn M, Kohlhof P, Hovestadt V, Johann P, Kool M, Pajtler KW, Korshunov A, Ruland V, Sperveslage J, Thomas C, Witt H, von Deimling A, Paulus W, Pfister SM, Capper D, Hasselblatt M |title=Papillary Tumor of the Pineal Region: A Distinct Molecular Entity |journal=Brain Pathol |volume=26 |issue=2 |pages=199–205 |date=March 2016 |pmid=26113311 |doi=10.1111/bpa.12282 |url=}}</ref> | |||
*Chromosome 10 loss. | |||
DDx: | DDx: | ||
| Line 147: | Line 154: | ||
*Males > females. | *Males > females. | ||
*Children & young adults. | *Children & young adults. | ||
*Corresponds to WHO IV (ICD-O: 9362/3) | *Corresponds to WHO IV (ICD-O: 9362/3). | ||
*May be a manifestation of the [[DICER1 syndrome]].<ref name=pmid28960912>{{Cite journal | last1 = van Engelen | first1 = K. | last2 = Villani | first2 = A. | last3 = Wasserman | first3 = JD. | last4 = Aronoff | first4 = L. | last5 = Greer | first5 = MC. | last6 = Tijerin Bueno | first6 = M. | last7 = Gallinger | first7 = B. | last8 = Kim | first8 = RH. | last9 = Grant | first9 = R. | title = DICER1 syndrome: Approach to testing and management at a large pediatric tertiary care center. | journal = Pediatr Blood Cancer | volume = 65 | issue = 1 | pages = | month = Jan | year = 2018 | doi = 10.1002/pbc.26720 | PMID = 28960912 }}</ref> | |||
===Microscopic=== | ===Microscopic=== | ||
| Line 162: | Line 170: | ||
*Synaptophysin+ve | *Synaptophysin+ve | ||
*MIB-1: high. | *MIB-1: high. | ||
===Molecular=== | |||
* DICER1 mutations.<ref name="pmid25022261">{{cite journal |authors=de Kock L, Sabbaghian N, Druker H, Weber E, Hamel N, Miller S, Choong CS, Gottardo NG, Kees UR, Rednam SP, van Hest LP, Jongmans MC, Jhangiani S, Lupski JR, Zacharin M, Bouron-Dal Soglio D, Huang A, Priest JR, Perry A, Mueller S, Albrecht S, Malkin D, Grundy RG, Foulkes WD |title=Germ-line and somatic DICER1 mutations in pineoblastoma |journal=Acta Neuropathol |volume=128 |issue=4 |pages=583–95 |date=October 2014 |pmid=25022261 |pmc=4381868 |doi=10.1007/s00401-014-1318-7 |url=}}</ref> | |||
*DROSHA deletions. <ref name="pmid30877433">{{cite journal |authors=Lee JC, Mazor T, Lao R, Wan E, Diallo AB, Hill NS, Thangaraj N, Wendelsdorf K, Samuel D, Kline CN, Banerjee A, Auguste K, Raffel C, Gupta N, Berger M, Raleigh DR, Shai A, Phillips JJ, Bollen AW, Tihan T, Perry A, Costello J, Solomon DA |title=Recurrent KBTBD4 small in-frame insertions and absence of DROSHA deletion or DICER1 mutation differentiate pineal parenchymal tumor of intermediate differentiation (PPTID) from pineoblastoma |journal=Acta Neuropathol |volume=137 |issue=5 |pages=851–854 |date=May 2019 |pmid=30877433 |pmc=6483828 |doi=10.1007/s00401-019-01990-5 |url=}}</ref> | |||
DDx: | DDx: | ||
Latest revision as of 17:20, 25 March 2021
The pineal gland is thingy that is most noted for the fact that it calcifies with age.
Normal histology
- Cellular.
Overview
Non-neoplastic:
- Cysts
Tumours:[1]
- Primary pineal tumours ~15% of (pineal) tumours - benign to malignant:[2]
- Pineocytoma.
- Pineal parenchymal tumor of intermediate differentiation.
- Pineoblastoma.
- Germ cell tumours:
- Germinoma ~ 50% of (pineal) tumours.
- Teratoma ~ 15% of tumours.
- Choriocarcinoma ~ 5% of tumours.
- Others:
- Direct invasion/extension from surrounding structures (astrocytomas).
- Metastases.
- Lipomas.
- Meningiomas.
Pineal gland cyst
Pineocytoma
General
- Benign tumour of the pineal gland.
- WHO Grade I.
Microscopic
Features:
- Cytologically benign cells (uniform size of nuclei, regular nuclear membrane, light chromatin).
- Pineocytomatous/neurocytic rosette = (irregular) rosette with a large meshwork of fibers (neuropil) at the centre.[5]
- Similar to Homer-Wright rosette... but:
- Neuropil centre is larger in pineocytoma.
- Edge of neuropil meshwork irregular.
- Similar to Homer-Wright rosette... but:
Notes:
- Rosette = circular/flower-like arrangement of cells.
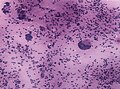
Images
IHC
- Synaptophysin +ve.
- Chromogranin A -ve.
- NSE +ve (cytoplasmic + nuclear).[6]
- GFAP -ve.
- +ve in gliomas.
- PLAP -ve.
- Usu. +ve in germ cell tumours.
- Ki-67.
Another ref.:[7]
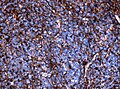
Pineal parenchymal tumor of intermediate differentiation
General
- 20% of all pineal tumors.
- Affects all ages.
- ICD-O: 9362/3
- No WHO grade yet, clinical behaviour corresponds to grade II/III[8]
Microscopic
Features:[9]
- High cellularity.
- Mild to moderate atypia.
- Mitoses.
- Usually no pinecytomatous rosettes.
- High pleomorphism possible.
Molecular
- Insertions in KBTBD4.[10]
Images:
Papillary tumour of pineal region (PTPR)
General
- Very rare neuoepithelial tumor of adults.
- Proposed ICD-O: 9395/3
- No WHO grade yet, clinical behaviour corresponds to grade II/III[11]
Gross:
- Well circumscribed.
- Can be quite large (2-4cm).
- Macroscopy mimics pineocytoma.
Microscopic
Features:[12]
- Papillary growth pattern.
- Dense areas exhibit ependymal features.
- Clear, vacuolated cytoplasm.
- Rosettes.
- Round to oval nuclei.
- Mitoses (0-10/HPF).
- Necroses.
- Hyalinized vessels.
IHC
- +ve for keratins (KL1, AE1/AE3, Cam5.2, CK18).
- GFAP and Synaptophysin focally +ve.
- S100+ve.
- EMA mostly -ve.
- NF and Kir 7.1-ve.
Molecular
- PTEN alterations. [13]
- Chromosome 10 loss.
DDx: Ependymoma.
Images:
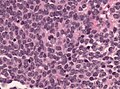
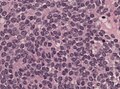
Pineoblastoma
General
- Rare.
- Malignant.
- Males > females.
- Children & young adults.
- Corresponds to WHO IV (ICD-O: 9362/3).
- May be a manifestation of the DICER1 syndrome.[14]
Microscopic
Features:
- Hypercellular.
- Mitoses.
- Nuclear atypia.
- Homer-wright & Flexner-Winterstein rosettes
- Fleurettes.
IHC
- GFAP -ve/+ve.
- NF+ve.
- Synaptophysin+ve
- MIB-1: high.
Molecular
DDx:
- Glioblastoma, small cell variant.
- Small round cell tumors.
Images:
See also
References
- ↑ Gaillard F, Jones J (October 2010). "Masses of the pineal region: clinical presentation and radiographic features". Postgrad Med J 86 (1020): 597–607. doi:10.1136/pgmj.2009.087460. PMID 20971711.
- ↑ Smith AB, Rushing EJ, Smirniotopoulos JG (November 2010). "From the archives of the AFIP: lesions of the pineal region: radiologic-pathologic correlation". Radiographics 30 (7): 2001–20. doi:10.1148/rg.307105131. PMID 21057132.
- ↑ Pu, Y.; Mahankali, S.; Hou, J.; Li, J.; Lancaster, JL.; Gao, JH.; Appelbaum, DE.; Fox, PT. (Oct 2007). "High prevalence of pineal cysts in healthy adults demonstrated by high-resolution, noncontrast brain MR imaging.". AJNR Am J Neuroradiol 28 (9): 1706-9. doi:10.3174/ajnr.A0656. PMID 17885233.
- ↑ Mena, H.; Armonda, RA.; Ribas, JL.; Ondra, SL.; Rushing, EJ. (Oct 1997). "Nonneoplastic pineal cysts: a clinicopathologic study of twenty-one cases.". Ann Diagn Pathol 1 (1): 11-8. PMID 9869821.
- ↑ Wippold FJ, Perry A (March 2006). "Neuropathology for the neuroradiologist: rosettes and pseudorosettes". AJNR Am J Neuroradiol 27 (3): 488–92. PMID 16551982.
- ↑ URL: http://path.upmc.edu/cases/case157/dx.html. Accessed on: 9 December 2010.
- ↑ URL: http://www.springerlink.com/content/k4v88n6h6jknhp2t/fulltext.pdf. Accessed on: 9 December 2010.
- ↑ Jouvet, A.; Saint-Pierre, G.; Fauchon, F.; Privat, K.; Bouffet, E.; Ruchoux, MM.; Chauveinc, L.; Fèvre-Montange, M. (Jan 2000). "Pineal parenchymal tumors: a correlation of histological features with prognosis in 66 cases.". Brain Pathol 10 (1): 49-60. PMID 10668895.
- ↑ Fèvre-Montange, M.; Szathmari, A.; Champier, J.; Mokhtari, K.; Chrétien, F.; Coulon, A.; Figarella-Branger, D.; Polivka, M. et al. (Jul 2008). "Pineocytoma and pineal parenchymal tumors of intermediate differentiation presenting cytologic pleomorphism: a multicenter study.". Brain Pathol 18 (3): 354-9. doi:10.1111/j.1750-3639.2008.00128.x. PMID 18371183.
- ↑ Pfaff E, Aichmüller C, Sill M, Stichel D, Snuderl M, Karajannis MA, Schuhmann MU, Schittenhelm J, Hasselblatt M, Thomas C, Korshunov A, Rhizova M, Wittmann A, Kaufhold A, Iskar M, Ketteler P, Lohmann D, Orr BA, Ellison DW, von Hoff K, Mynarek M, Rutkowski S, Sahm F, von Deimling A, Lichter P, Kool M, Zapatka M, Pfister SM, Jones DTW (February 2020). "Molecular subgrouping of primary pineal parenchymal tumors reveals distinct subtypes correlated with clinical parameters and genetic alterations". Acta Neuropathol 139 (2): 243–257. doi:10.1007/s00401-019-02101-0. PMID 31768671.
- ↑ Fèvre-Montange, M.; Hasselblatt, M.; Figarella-Branger, D.; Chauveinc, L.; Champier, J.; Saint-Pierre, G.; Taillandier, L.; Coulon, A. et al. (Oct 2006). "Prognosis and histopathologic features in papillary tumors of the pineal region: a retrospective multicenter study of 31 cases.". J Neuropathol Exp Neurol 65 (10): 1004-11. doi:10.1097/01.jnen.0000240462.80263.13. PMID 17021405.
- ↑ Heim, S.; Beschorner, R.; Mittelbronn, M.; Keyvani, K.; Riemenschneider, MJ.; Vajtai, I.; Hartmann, C.; Acker, T. et al. (Jan 2014). "Increased mitotic and proliferative activity are associated with worse prognosis in papillary tumors of the pineal region.". Am J Surg Pathol 38 (1): 106-10. doi:10.1097/PAS.0b013e31829e492d. PMID 24121176.
- ↑ Heim S, Sill M, Jones DT, Vasiljevic A, Jouvet A, Fèvre-Montange M, Wesseling P, Beschorner R, Mittelbronn M, Kohlhof P, Hovestadt V, Johann P, Kool M, Pajtler KW, Korshunov A, Ruland V, Sperveslage J, Thomas C, Witt H, von Deimling A, Paulus W, Pfister SM, Capper D, Hasselblatt M (March 2016). "Papillary Tumor of the Pineal Region: A Distinct Molecular Entity". Brain Pathol 26 (2): 199–205. doi:10.1111/bpa.12282. PMID 26113311.
- ↑ van Engelen, K.; Villani, A.; Wasserman, JD.; Aronoff, L.; Greer, MC.; Tijerin Bueno, M.; Gallinger, B.; Kim, RH. et al. (Jan 2018). "DICER1 syndrome: Approach to testing and management at a large pediatric tertiary care center.". Pediatr Blood Cancer 65 (1). doi:10.1002/pbc.26720. PMID 28960912.
- ↑ de Kock L, Sabbaghian N, Druker H, Weber E, Hamel N, Miller S, Choong CS, Gottardo NG, Kees UR, Rednam SP, van Hest LP, Jongmans MC, Jhangiani S, Lupski JR, Zacharin M, Bouron-Dal Soglio D, Huang A, Priest JR, Perry A, Mueller S, Albrecht S, Malkin D, Grundy RG, Foulkes WD (October 2014). "Germ-line and somatic DICER1 mutations in pineoblastoma". Acta Neuropathol 128 (4): 583–95. doi:10.1007/s00401-014-1318-7. PMC 4381868. PMID 25022261. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4381868/.
- ↑ Lee JC, Mazor T, Lao R, Wan E, Diallo AB, Hill NS, Thangaraj N, Wendelsdorf K, Samuel D, Kline CN, Banerjee A, Auguste K, Raffel C, Gupta N, Berger M, Raleigh DR, Shai A, Phillips JJ, Bollen AW, Tihan T, Perry A, Costello J, Solomon DA (May 2019). "Recurrent KBTBD4 small in-frame insertions and absence of DROSHA deletion or DICER1 mutation differentiate pineal parenchymal tumor of intermediate differentiation (PPTID) from pineoblastoma". Acta Neuropathol 137 (5): 851–854. doi:10.1007/s00401-019-01990-5. PMC 6483828. PMID 30877433. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6483828/.