Difference between revisions of "Pericardium"
Jump to navigation
Jump to search
| Line 7: | Line 7: | ||
*Infectious pericarditis - post-procedural. | *Infectious pericarditis - post-procedural. | ||
*[[Fibrinous pericarditis]]. | *[[Fibrinous pericarditis]]. | ||
*Pericardial cyst. | *[[Pericardial cyst]]. | ||
===Malignant=== | ===Malignant=== | ||
Latest revision as of 12:12, 8 July 2016
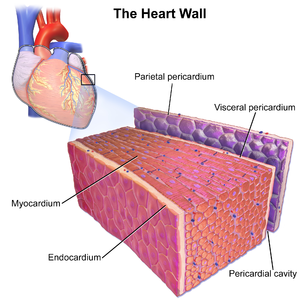
Pericardium is a specimen that uncommonly comes to pathology.
Pathologies of the pericardium
Benign
- Idiopathic pericarditis - common.[1]
- Infectious pericarditis - post-procedural.
- Fibrinous pericarditis.
- Pericardial cyst.
Malignant
Related pathologies
- Pericardial effusion.
- Hemopericardium.
- Cardiac tamponade.
Specific entities
Idiopathic pericarditis
- Pericarditis redirects here.
General
- Uncommon.
- In the clinical context pericarditis is used for things that probably don't have inflammation.[2]
- "Pericardial heart disease" may be a better descriptor.
Etiologies of pericarditis:[3]
- Infectious:
- Fungal.
- Bacterial.
- Idiopathic - most common.
- Neoplastic.
- Autoimmune, e.g. systemic lupus erythematosus.
- Uremia - chronic renal failure.
- Traumatic - post-surgical.
- Associated with myocardial infarction - Dressler's syndrome.
Gross
Features:[3]
- Thickening.
- +/-Pericardial effusion.
Notes:
- Normal pericardial fluid volume 5-35 mL.[3]
Microscopic
Features:
- Inflammatory cells:
- Neutrophils.
- Lymphocytes.
- Plasma cells.
- +/-Hemosiderin-laden macrophages.
DDx:
- Infectious pericarditis.
- Malignant mesothelioma.[1]
Images
Sign out
PERICARDIUM, BIOPSY: - ACUTE AND CHRONIC PERICARDITIS WITH SIDEROPHAGES AND REACTIVE MESOTHELIAL CHANGES. - NO MICRO-ORGANISMS SEEN WITH ROUTINE STAINING. - NO EVIDENCE OF MALIGNANCY.
Micro
The sections show fibrous tissue with minimal adipose tissue that is covered by mesothelium. A mixed inflammatory infiltrate is present that consists primarily of lymphocytes and plasma cells. Rare eosinophils are seen. Focally, neutrophils are seen and associated with reactive mesothelial cells. Abundant hemosideratin-laden macrophages are seen. No fibrinous strands are seen. No significant nuclear atypia is identified and no atypical infiltrative cell population is identified. No micro-organisms are identified with routine staining.
See also
References
- ↑ 1.0 1.1 Smets P, Guettrot-Imbert G, Hermet M, et al. (September 2013). "[Recurrent pericarditis related to primary pericardial malignant mesothelioma]" (in French). Rev Med Interne 34 (9): 573–6. doi:10.1016/j.revmed.2013.04.021. PMID 23773902.
- ↑ Roberts, WC. (Jan 2005). "Pericardial heart disease: its morphologic features and its causes.". Proc (Bayl Univ Med Cent) 18 (1): 38-55. PMID 16200146.
- ↑ 3.0 3.1 3.2 Peebles CR, Shambrook JS, Harden SP (December 2011). "Pericardial disease--anatomy and function". Br J Radiol 84 Spec No 3: S324–37. doi:10.1259/bjr/16168253. PMC 3473919. PMID 22723538. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3473919/.