Difference between revisions of "Dermatopathology"
(→Leukoplakia: update) |
Alessandro (talk | contribs) m (two typos) |
||
| (109 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
'''Dermatopathology''' is the pathology of skin. | '''Dermatopathology''' is the pathology of skin. | ||
Pathology is a significant part of dermatology and dermatologists spend five years in residency. So, it is a huge area. | Pathology is a significant part of dermatology and dermatologists spend five years in residency. So, it is a huge area. | ||
=Specimens= | |||
*Shave biopsy = done for what is presumed to be benign disease - classically exophytic lesions, e.g. [[seborrheic keratosis]]. | |||
*Saucerization = scooped shave biopsy.<ref>{{Cite journal | last1 = Elston | first1 = D. | title = Practical advice regarding problematic pigmented lesions. | journal = J Am Acad Dermatol | volume = 67 | issue = 1 | pages = 148-55 | month = Jul | year = 2012 | doi = 10.1016/j.jaad.2012.04.006 | PMID = 22703907 }} | |||
</ref> | |||
*Punch biopsy = cylindrical piece of skin, usu. epidermis and dermis - suspicious lesions/malignant lesions, e.g. [[basal cell carcinoma]]. | |||
*Incisional biopsy = a piece of the lesion for pathologic assessment; lesion not completely removed. | |||
*Excision = lesion cut-out with intent for complete removal - usual has a generous margin, e.g. [[malignant melanoma]] excision. | |||
*Re-excision = done to get a wider margin ''or'' remove part of a lesion that was incompletely removed in a prior excision. | |||
**Conservative re-excision = cut-out more with a minimal rim of normal tissue.<ref>URL: [http://www.nedermatology.com/skin-cancer-treatments.php http://www.nedermatology.com/skin-cancer-treatments.php]. Accessed on: 26 February 2013.</ref> | |||
*[[Sentinel lymph node]] removal = a special type of lymphadenectomy usu. done for [[cancer staging|staging]], esp. [[malignant melanoma]]. | |||
=Histology= | =Histology= | ||
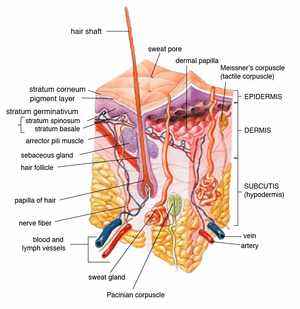
==Layers of the skin== | ==Layers of the skin== | ||
[[Image:Skin.png|thumb|Schematic showing the layers and structures of skin. (WC/cancer.gov)]] | |||
*Epidermis - outer most layer, avascular, separated from dermis by a basement membrane, epithelial tissue. | *Epidermis - outer most layer, avascular, separated from dermis by a basement membrane, epithelial tissue. | ||
*Dermis - below the epidermis, vascular, separated from the epidermis by a basement membrane, connective tissue. | *Dermis - below the epidermis, vascular, separated from the epidermis by a basement membrane, connective tissue. | ||
==Epidermis== | Note: | ||
*The layer below the skin is the ''subdermis'' ([[AKA]] hypodermis, [[AKA]] subcutaneous tissue). | |||
**It is below the dermis and consists of adipose tissue.<ref>URL: [http://histologyolm.stevegallik.org/node/119 http://histologyolm.stevegallik.org/node/119]. Accessed on: 5 November 2013.</ref> | |||
Image: | |||
*[http://histologyolm.stevegallik.org/node/119 Dermis and hypodermis (stevegallik.org)]. | |||
===Epidermis=== | |||
====Layers of the epidermis==== | |||
[[Image:Epidermal layers.png|thumb|right|Layers of the epidermis. (WC/Wbensmith)]] | |||
Epidermis layers - from the surface to epidermal-dermal junction: | Epidermis layers - from the surface to epidermal-dermal junction: | ||
*Stratum corneum. | *Stratum corneum. | ||
| Line 19: | Line 39: | ||
Mnemonic: ''Corn Lovers Grow Several Bales''. | Mnemonic: ''Corn Lovers Grow Several Bales''. | ||
===Cells of the epidermis=== | ====Cells of the epidermis==== | ||
*Keratinocytes. | *Keratinocytes. | ||
** | **Usually eosinophilic cytoplasm - '''important feature'''. | ||
**May have clear perinuclear halo (glycogenated keratinocytes). | **May have clear perinuclear halo (glycogenated keratinocytes). | ||
**Intercellular bridges (high power) - '''key feature'''. | **Intercellular bridges (high power) - '''key feature'''. | ||
*Melanocytes. | *Melanocytes. | ||
** | **Usuallly basal location. | ||
**Epithelioid or | **Epithelioid or dendritic morphology. | ||
**Pericellular clearing - '''key feature'''. | **Pericellular clearing - '''key feature'''. | ||
**Clear cytoplasm. | **Clear cytoplasm. | ||
| Line 40: | Line 60: | ||
***[[Paget disease]]: large cells with clear cytoplasm, may cluster, above basal layer. | ***[[Paget disease]]: large cells with clear cytoplasm, may cluster, above basal layer. | ||
==Adnexal structures== | ====Normal histology==== | ||
Features: | |||
*Keratinocytes: | |||
**Basal ~ 2x [[RBC]]. | |||
***May palisade focally ~ 1:2 = width: height. | |||
*Melanocytes < 25 melanocytes / 0.5 mm of basal layer.<ref name=pmid21549242>{{Cite journal | last1 = Trotter | first1 = MJ. | title = Melanoma margin assessment. | journal = Clin Lab Med | volume = 31 | issue = 2 | pages = 289-300 | month = Jun | year = 2011 | doi = 10.1016/j.cll.2011.03.006 | PMID = 21549242 }}</ref> | |||
*Basket weave stratum corneum (non-acral skin). | |||
===Dermis=== | |||
Subdivided into layers: | |||
#Papillary dermis. | |||
#*Location: superficial - opposed to the deep aspect of the epidermis. | |||
#*Appearance: dense, thick collagen bundles. | |||
#Reticular dermis. | |||
#*Location: deep - between papillary dermis and subdermis. | |||
#*Appearance: loose connective tissue. | |||
Images: | |||
*[http://www.biology-online.org/user_files/Image/Anatomy/AN-fibroblastF02.gif Layers of the dermis - labelled (biology-online.org)].<ref>URL: [http://www.biology-online.org/articles/fibroblast_heterogeneity_skin_deep/figures.html http://www.biology-online.org/articles/fibroblast_heterogeneity_skin_deep/figures.html]. Accessed on: 29 March 2012.</ref> | |||
*[http://melanoma.blogsome.com/wp-admin/images/skinstr.jpg Layers of the skin (melanoma.blogsome.com)].<ref>URL: [http://melanoma.blogsome.com/category/skin-structure/ http://melanoma.blogsome.com/category/skin-structure/]. Accessed on: 29 March 2012.</ref> | |||
===Adnexal structures=== | |||
The top five structures of the skin:<ref>{{Ref Derm|4-8}}</ref> | The top five structures of the skin:<ref>{{Ref Derm|4-8}}</ref> | ||
{| class="wikitable" | {| class="wikitable sortable" | ||
! Structure / Attribute | |||
! Histomorphology | |||
! Function | |||
! [[IHC]] | |||
! Other | |||
! Image | |||
|- | |- | ||
| '''Eccrine gland''' | | '''Eccrine gland''' | ||
| clusters of tubular structures, pale cytoplasm | | clusters of tubular structures, pale cytoplasm | ||
| thermoregulation (cooling) - produce sweat | | thermoregulation (cooling) - produce sweat | ||
| CK7+, CEA+, CAM5.2+, EMA+ | | [[CK7]]+, [[CEA]]+, CAM5.2+, [[EMA]]+ | ||
| ? | | ? | ||
| ? | | ? | ||
| Line 80: | Line 121: | ||
| '''Nail''' | | '''Nail''' | ||
| epidermal structure | | epidermal structure | ||
| | | weapon (claw-like), look pretty? | ||
| ? | | ? | ||
| ? | | ? | ||
| [http://histology.osumc.edu/histology/HumanHisto/Integumentary/Img/17B-23_001.html (osumc.edu)], [http://ctrgenpath.net/static/atlas/mousehistology/Windows/integumentary/nail20.html (ctrgenpath.net)] | |||
|- | |- | ||
|} | |} | ||
| Line 92: | Line 133: | ||
=Common terms= | =Common terms= | ||
==Clinical descriptors== | |||
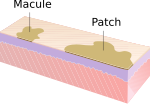
There are multitude of clinical descriptors - common ones are:<ref>URL: [http://www.pediatrics.wisc.edu/education/derm/text.html http://www.pediatrics.wisc.edu/education/derm/text.html]. Accessed on: 18 September 2012.</ref> | |||
{| class="wikitable sortable" | |||
! '''Name''' | |||
! '''Size †''' | |||
! '''Description''' | |||
! '''Other''' | |||
! '''Image''' | |||
|- | |||
| Macule | |||
| <= 10 mm | |||
| flat + change of colour | |||
| if > 10 mm --> patch | |||
| [[Image:Macule_and_Patch.svg|thumb|center|150px| Macule (WC)]] | |||
|- | |||
| Patch | |||
| > 10 mm | |||
| flat + change of colour | |||
| if <= 10 mm --> macule | |||
| [[Image:Macule_and_Patch.svg|thumb|center|150px| Patch (WC)]] | |||
|- | |||
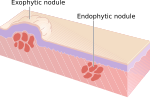
| Papule | |||
| <= 10 mm | |||
| raised | |||
| if > 10 mm --> nodule | |||
| [[Image:Papule_and_Plaque.svg|thumb|center|150px| Papule (WC)]] | |||
|- | |||
| Nodule | |||
| > 10 mm | |||
| raised | |||
| if <= 10 mm --> papule | |||
| [[Image:Nodules.svg|thumb|center|150px| Nodule (WC)]] | |||
|- | |||
| Plaque | |||
| > 10 mm | |||
| raised, flat-top | |||
| plateau-like | |||
| [[Image:Papule_and_Plaque.svg|thumb|center|150px| Plaque (WC)]] | |||
|- | |||
| Vesicle | |||
| <= 10 mm | |||
| raised, fluid filled | |||
| if > 10 mm --> bulla | |||
| [[Image:Vesicles_and_Bulla.svg |thumb|center|150px| Vesicle (WC)]] | |||
|- | |||
| Bulla | |||
| > 10 mm | |||
| raised, fluid filled | |||
| if <= 10 mm --> vesicle | |||
| [[Image:Vesicles_and_Bulla.svg |thumb|center|150px| Bulla (WC)]] | |||
|} | |||
Note: | |||
* † Definitions vary -- some authors use a 5 mm cut-off. | |||
==Histologic descriptors== | |||
Dermatopathology doesn't have intuitive terms, e.g. thickening of the stratum spinosum isn't ''spinosum hyperplasia''. The terms have to committed to memory. | |||
===Common terms in a table=== | |||
{| class="wikitable sortable" | |||
! Term | |||
! Meaning | |||
! Reference | |||
|- | |||
|Acanthosis | |||
| thickening of the prickle layer (stratum spinosum) of epidermis | |||
| <ref>[http://dictionary.reference.com/browse/acanthosis http://dictionary.reference.com/browse/acanthosis]</ref> | |||
|- | |||
|Acantholysis | |||
| loss of intercellular connections in the epidermis | |||
| | |||
|- | |||
|Dyskeratosis | |||
| abnormal keratinization, often refers to keratinization below the stratum granulosum; keratinization above may be abnormal (dependent on body site) | |||
| | |||
|- | |||
|Parakeratosis | |||
| retention of nuclei in the stratum corneum, normal in mucous membranes | |||
| | |||
|- | |||
|Spongiosis | |||
| epidermal intercellular edema; cells appear to have a clear halo around 'em | |||
| <ref>{{Ref PBoD|1230}}</ref> | |||
|- | |||
|Basketweave stratum corneum | |||
| appearance of the normal stratum corneum; presence in the context of pathology suggests an acute process | |||
| | |||
|- | |||
|Compact hyperkeratosis | |||
| stratum corneum layer is dense and thickened; this suggests a chronic process | |||
| <ref>URL: [http://dermnetnz.org/pathology/pathology-glossary.html http://dermnetnz.org/pathology/pathology-glossary.html]. Accessed on: 8 August 2012.</ref> | |||
|- | |||
| Hyperkeratosis | |||
| thickened stratum corneum - also see ''compact hyperkeratosis'' and ''basketweave stratum corneum'' | |||
| | |||
|- | |||
|Epidermotropism † | |||
| intraepithelial lymphocytes in [[CTCL]]; how to remember: epidermotropis''m'' = ''m''alignant | |||
| <ref name=pmid20132423>{{Cite journal | last1 = Fung | first1 = MA. | title = 'Epidermotropism' vs. 'exocytosis' of lymphocytes 101: definition of terms. | journal = J Cutan Pathol | volume = 37 | issue = 5 | pages = 525-9 | month = May | year = 2010 | doi = 10.1111/j.1600-0560.2010.01515.x | PMID = 20132423 }}</ref> | |||
|- | |||
|Exocytosis † | |||
| intraepithelial lymphocytes in benign conditions | |||
| <ref name=pmid20132423>{{Cite journal | last1 = Fung | first1 = MA. | title = 'Epidermotropism' vs. 'exocytosis' of lymphocytes 101: definition of terms. | journal = J Cutan Pathol | volume = 37 | issue = 5 | pages = 525-9 | month = May | year = 2010 | doi = 10.1111/j.1600-0560.2010.01515.x | PMID = 20132423 }}</ref> | |||
|- | |||
|Orthokeratosis | |||
| anuclear keratin layer is present (stratum corneum) - seen in normal skin; ''ortho-'' means ''correct'' | |||
| <ref>URL: [http://www.medilexicon.com/medicaldictionary.php?t=63448 http://www.medilexicon.com/medicaldictionary.php?t=63448]. Accessed on: 13 March 2013.</ref><ref>URL: [http://dictionary.reference.com/browse/ortho- http://dictionary.reference.com/browse/ortho-]. Accessed on: 13 March 2013.</ref> | |||
|} | |||
Note: | |||
* † These definitions are not universally accepted. ''Epidermotropism'' is sometimes used in the context of benign disease.<ref name=pmid9537476>{{Cite journal | last1 = Fung | first1 = MA. | last2 = LeBoit | first2 = PE. | title = Light microscopic criteria for the diagnosis of early vulvar lichen sclerosus: a comparison with lichen planus. | journal = Am J Surg Pathol | volume = 22 | issue = 4 | pages = 473-8 | month = Apr | year = 1998 | doi = | PMID = 9537476 }}</ref> | |||
Image: | |||
*[http://commons.wikimedia.org/wiki/File:Spongiotic_dermatitis_%282%29_Dyshidrotic_.JPG Spongiosis (WC)]. | *[http://commons.wikimedia.org/wiki/File:Spongiotic_dermatitis_%282%29_Dyshidrotic_.JPG Spongiosis (WC)]. | ||
===Others terms=== | |||
*Crust = epithelial elements, blood. | |||
Image: | |||
*[http://www.eplasty.com/article_images/eplasty10e60_fig3.gif Crust (eplasty.com)].<ref>URL: [http://www.eplasty.com/index.php?option=com_content&view=article&id=492&catid=171:volume-10-eplasty-2010&Itemid=121 http://www.eplasty.com/index.php?option=com_content&view=article&id=492&catid=171:volume-10-eplasty-2010&Itemid=121]. Accessed on: 16 October 2012.</ref> | |||
=Skin diseases= | =Skin diseases= | ||
| Line 109: | Line 261: | ||
*[[Basal cell carcinoma]] (BCC). | *[[Basal cell carcinoma]] (BCC). | ||
*[[Malignant melanoma]]. | *[[Malignant melanoma]]. | ||
* | *Metastases. | ||
==Non-malignant disease== | ==Non-malignant disease== | ||
| Line 141: | Line 293: | ||
| [[fibroepithelial polyp]] | | [[fibroepithelial polyp]] | ||
| Leser–Trélat sign = many SKs in malignancy | | Leser–Trélat sign = many SKs in malignancy | ||
| [ | | [[Image:Seborrheic_keratosis_(1).jpg |thumb|center|150px| SK (WC)]] | ||
|- | |- | ||
| [[Dermatofibroma]] | | [[Dermatofibroma]] | ||
| Line 150: | Line 302: | ||
| [[DFSP]] | | [[DFSP]] | ||
| very common | | very common | ||
| [ | | [[Image:SkinTumors-P9280848.jpg|thumb|center|150px|DF (WC)]] | ||
|- | |- | ||
| [[Fibroepithelial polyp]] (skin tag) | | [[Fibroepithelial polyp]] (skin tag) | ||
| Line 159: | Line 311: | ||
| [[seborrheic keratosis]] | | [[seborrheic keratosis]] | ||
| very common | | very common | ||
| [ | | [[Image:SkinTumors-P9250819.jpg|thumb|center|150px|Skin tag (WC)]] | ||
|- | |- | ||
| [[Lipoma]] | | [[Lipoma]] | ||
| Line 168: | Line 320: | ||
| [[liposarcoma]] | | [[liposarcoma]] | ||
| variants: angiolipoma (blood vessels), myolipoma (muscle) | | variants: angiolipoma (blood vessels), myolipoma (muscle) | ||
| [ | | [[Image: Lipoma -- high mag.jpg|thumb|center|150px|Lipoma (WC)]] | ||
|- | |- | ||
| [[Cicatrix]] (dermal scar) | | [[Cicatrix]] (dermal scar) | ||
| Line 174: | Line 326: | ||
| loss of adnexal structures, +/-[[giant cells]], +/-foreign material, +/-inflammatory cells | | loss of adnexal structures, +/-[[giant cells]], +/-foreign material, +/-inflammatory cells | ||
| site of previous trauma/surgery | | site of previous trauma/surgery | ||
| usu. none | | usu. none; S-100 (to exclude melanoma) | ||
| residual disease, [[hypertrophic scar]] | | residual disease, [[hypertrophic scar]], (desmoplastic) [[melanoma]] | ||
| | | | ||
| [ | | [[Image:ScarHistology.JPG |thumb|center|150px| Scar (WC)]] | ||
|- <!-- | |- <!-- | ||
| Entity | | Entity | ||
| Line 202: | Line 354: | ||
| [[Neurofibroma]] | | [[Neurofibroma]] | ||
| bland spindle cells | | bland spindle cells | ||
| mixed with collagen | | mast cells, mixed with collagen, assoc. with a nerve | ||
| may be associated with [[neurofibromatosis]] | | may be associated with [[neurofibromatosis]], esp. plexiform type | ||
| S100+ | | S100+, GFAP+ | ||
| | | neurotized [[melanocytic nevus]] | ||
| | | may develop into [[MPNST]] | ||
| [ | | [[Image:Neurofibroma_%281%29.jpg |thumb|center|150px| Neurofibroma (WC)]] | ||
|- | |- | ||
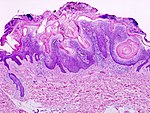
| [[Keratoacanthoma]] | | [[Keratoacanthoma]] | ||
| Line 216: | Line 368: | ||
| [[squamous cell carcinoma]] | | [[squamous cell carcinoma]] | ||
| some don't believe in the entity | | some don't believe in the entity | ||
| [ | | [[Image:Skin_keratoacanthoma_whole_slide.jpg |thumb|center|150px| Keratoacathoma (WC)]] | ||
|- | |- | ||
| [[Molluscum contagiosum]] | | [[Molluscum contagiosum]] | ||
| suprabasilar cells with abundant granular eosinophilic cytoplasm | | suprabasilar cells with abundant granular eosinophilic cytoplasm | ||
| small peripheral nucleus | | small peripheral nucleus | ||
| polypoid lesion (?) | | polypoid lesion; mushroom-like (?) | ||
| none (?) | | none (?) | ||
| DDx (?) | | DDx (?) | ||
| favourite exam case | | favourite exam case | ||
| [ | | [[Image:Molluscum_contagiosum_high_mag.jpg |thumb|center|150px|Molluscum contagiosum (WC)]] | ||
|- | |- | ||
| [[Verruca vulgaris]] | | [[Verruca vulgaris]] | ||
| Line 232: | Line 384: | ||
| raised lesions, classically on hand | | raised lesions, classically on hand | ||
| none (p16+?) | | none (p16+?) | ||
| | | [[squamous cell carcinoma of the skin|squamous cell carcinoma]] | ||
| caused by [[HPV]] | | caused by [[HPV]] | ||
| [ | | [[Image:Verruca_vulgaris_-_very_low_mag.jpg |thumb|center|150px| Verruca vulgaris (WC)]] | ||
|- | |- | ||
| [[Condyloma acuminatum]] | | [[Condyloma acuminatum]] | ||
| Line 241: | Line 393: | ||
| genital lesion | | genital lesion | ||
| none (p16+) | | none (p16+) | ||
| | | [[fibroepithelial polyp]] | ||
| | | caused by [[HPV]] | ||
| [ | | [[Image:Anal_condyloma_%282%29.jpg |thumb|center|150px| Condyloma acuminatum (WC)]] | ||
|- | |- | ||
| [[Granuloma annulare]] | | [[Granuloma annulare]] | ||
| dermal palisading [[granuloma]] around necrotic collagen | | dermal palisading [[granuloma]] around necrotic collagen | ||
| mucin in centre of lesion, (peripheral) | | mucin in centre of lesion, (peripheral) lymphocytes, usu. more superficial than necrobiosis lipoidica | ||
| benign, self-limited | | benign, self-limited | ||
| none (CD68?) | | none (CD68?) | ||
| [[necrobiosis lipoidica]], [[rheumatoid nodule]] | | [[necrobiosis lipoidica]], [[rheumatoid nodule]], [[epithelioid sarcoma]] | ||
| Other ? | | Other ? | ||
| [http://www. | | [[Image:Granuloma_annulare_-_add_-_high_mag.jpg |thumb|center|150px| GA (WC)]] | ||
|- | |||
| [[Necrobiosis lipoidica]] | |||
| dermal palisading [[granuloma]] around necrotic collagen, plasma cells | |||
| mucin in centre of lesion, (peripheral) chronic inflammatory cells | |||
| may be assoc. [[diabetes mellitus]] | |||
| none (CD68?) | |||
| [[granuloma annulare]], [[rheumatoid nodule]] | |||
| histology identical to ''necrobiosis lipoidica diabeticorum'' | |||
| [http://www.drmihm.com/cases/casefigure.cfm?figID=942&CaseID=53 (drmihm.com)] | |||
|- | |- | ||
| [[Angiofibroma]] | | [[Angiofibroma]] | ||
| Line 261: | Line 422: | ||
| DDx | | DDx | ||
| may be associated with [[tuberous sclerosis]] | | may be associated with [[tuberous sclerosis]] | ||
| [ | | [[Image:Nasopharyngeal angiofibroma - 2 - high mag.jpg|thumb|150px|Angiofibroma (WC)]] | ||
|- | |- | ||
| [[Keloid]] | | [[Keloid]] | ||
| Line 269: | Line 430: | ||
| none | | none | ||
| [[dermatofibroma]] (???) | | [[dermatofibroma]] (???) | ||
| hypertrophic scar | | [[hypertrophic scar]] | ||
| [ | | [[Image:Keloid_-_high_mag.jpg|thumb|center|150px|Keloid (WC)]] | ||
|- | |- | ||
| [[Eccrine poroma]] | | [[Eccrine poroma]] | ||
| Line 279: | Line 440: | ||
| DDx ? | | DDx ? | ||
| Other ? | | Other ? | ||
| [ | | [[Image:SkinTumors-P7150495.JPG|thumb|center|150px|EP (WC)]] | ||
|- | |- | ||
| [[Syringoma]] | | [[Syringoma]] | ||
| bilayered ducts, occasionally tadpole like shape | | bilayered ducts, occasionally tadpole like shape | ||
| | | | ||
| usu. close to eyelid | | usu. close to [[eyelid]] | ||
| Stains/IHC ? | | Stains/IHC ? | ||
| DDx ? | | DDx ? | ||
| Line 291: | Line 452: | ||
|- | |- | ||
| [[Chondroid syringoma]] (mixed tumour of skin) | | [[Chondroid syringoma]] (mixed tumour of skin) | ||
| chondromyxoid stroma, epithelial component | | [[chondromyxoid stroma]], epithelial component | ||
| epithelial component in nests with eosinophilic cytoplasm, round/ovoid nuclei with nucleoli | | epithelial component in nests with eosinophilic cytoplasm, round/ovoid nuclei with nucleoli | ||
| Clinical ? | | Clinical ? | ||
| Line 298: | Line 459: | ||
| related to [[pleomorphic adenoma]] (???) | | related to [[pleomorphic adenoma]] (???) | ||
| Image ? | | Image ? | ||
|- | |||
| [[Angiokeratoma]] | |||
| ectatic superficial dermal vessels + overlying hyperkeratosis | |||
| - | |||
| may be seen in [[Fabry disease]] | |||
| Stains/IHC ? | |||
| [[venous lake]] | |||
| Other ? | |||
| [[Image:Angiokeratoma_-_low_mag.jpg |thumb|center|150px| Angiokeratoma (WC)]] | |||
|- <!-- | |- <!-- | ||
| Entity | | Entity | ||
| Line 325: | Line 495: | ||
| common in children | | common in children | ||
| none | | none | ||
| | | [[squamous cell carcinoma of the skin|squamous cell carcinoma]] | ||
| mutations of CTNNB1 gene | | mutations of CTNNB1 gene | ||
| [ | | [[Image:Pilomatrixoma_-_intermed_mag.jpg |thumb|center|150px| Pilomatrixcoma (WC)]] | ||
|- | |- | ||
| [[Juvenile xanthogranuloma]] (JXG) | | [[Juvenile xanthogranuloma]] (JXG) | ||
| Line 336: | Line 506: | ||
| [[Langerhans cell histiocytosis]] | | [[Langerhans cell histiocytosis]] | ||
| may be seen in adults, known as '''adult xanthogranuloma''' | | may be seen in adults, known as '''adult xanthogranuloma''' | ||
| [ | | [[Image:Juvenile_xanthogranuloma_-_high_mag.jpg |thumb|center|150px| JXG (WC)]] | ||
|} | |} | ||
| Line 357: | Line 527: | ||
| [[pilar cyst]], [[dermoid cyst]] | | [[pilar cyst]], [[dermoid cyst]] | ||
| Other? | | Other? | ||
| [ | | [[Image:Epidermal inclusion cyst -- high mag.jpg |thumb|center|150px| Epidermal inclusion cyst (WC)]] | ||
|- | |- | ||
| [[Pilar cyst]] | | [[Pilar cyst]] (trichilemmal cyst) | ||
| cyst lined by squamous epithelium '''without''' a granular layer | | cyst lined by squamous epithelium '''without''' a granular layer | ||
| keratinous debris | | keratinous debris | ||
| Line 366: | Line 536: | ||
| [[epidermal cyst]] | | [[epidermal cyst]] | ||
| Other? | | Other? | ||
| Image | | [[Image:Trichilemmal_cyst_-_very_high_mag.jpg |thumb|center|100px| Pilar cyst (WC)]] | ||
|- | |- | ||
| [[Steatocystoma]] | | [[Steatocystoma]] | ||
| Line 375: | Line 545: | ||
| [[dermoid cyst]], follicular cyst | | [[dermoid cyst]], follicular cyst | ||
| Other? | | Other? | ||
| Image | | [[Image:Steatocystoma_-_high_mag.jpg |thumb|center|150px| Steatocystoma (WC)]] | ||
|- | |- | ||
| [[Dermoid cyst]] | | [[Dermoid cyst]] | ||
| Line 400: | Line 570: | ||
| [[Actinic keratosis]] | | [[Actinic keratosis]] | ||
| epidermal atypia, esp. (basal) nuclear enlargement | | epidermal atypia, esp. (basal) nuclear enlargement | ||
| var. of size, shape and staining | | var. of nuclear size, shape and staining, parakeratosis (important in early lesions); does ''not'' involves adnexal epithelium and follicular epithelium | ||
| yellow-brown scaly | | yellow-brown scaly | ||
| none | | none | ||
| [[squamous carcinoma]], [[Bowen disease]] | | [[squamous carcinoma]], [[Bowen disease]] | ||
| seen with [[solar elastosis]] | | seen with [[solar elastosis]] | ||
| [ | | [[Image:Actinic_Keratosis,_H%26E.jpg |thumb|center|150px| AK (WC)]] | ||
|- | |- | ||
| [[Bowen disease]] (squamous cell carcinoma in situ) | | [[Bowen disease]] (squamous cell carcinoma in situ) | ||
| epidermal atypia, esp. suprabasal nuclear enlargement | | epidermal atypia, esp. suprabasal nuclear enlargement | ||
| var. of size, shape and staining | | var. of nuclear size, shape and staining; usually full thickness involvement; involve adnexal epithelium and follicular epithelium | ||
| | | | ||
| none | | none | ||
| [[squamous carcinoma]], [[actinic keratosis]] | | [[squamous carcinoma]], [[actinic keratosis]] | ||
| typically seen with solar elastosis | | typically seen with solar elastosis | ||
| [ | | [[Image:Bowen_disease_%281%29.jpg |thumb|center|100px| Bowen's disease (WC)]] | ||
|} | |} | ||
| Line 430: | Line 600: | ||
| [[Basal cell carcinoma]] (BCC) | | [[Basal cell carcinoma]] (BCC) | ||
| basaloid cells with peripheral palisading, artificial cleft | | basaloid cells with peripheral palisading, artificial cleft | ||
| myxoid stroma | | [[myxoid]] stroma | ||
| raised, pearly, telangiectasia | | raised, pearly, telangiectasia | ||
| usu. none req., CK5/6+ | | usu. none req., [[CK5/6]]+ | ||
| [[trichoepithelioma]] | | [[trichoepithelioma]], [[basaloid squamous cell carcinoma]] | ||
| assoc. [[nevoid basal cell carcinoma syndrome]], Bazex syndrome | | assoc. [[nevoid basal cell carcinoma syndrome]], [[Bazex syndrome]] | ||
| [ | | [[Image:Basal cell carcinoma - high mag.jpg| thumb| center|150px|BCC (WC)]] | ||
|- | |- | ||
| [[Squamous cell carcinoma]] (SCC) | | [[Squamous cell carcinoma]] (SCC) | ||
| Line 442: | Line 612: | ||
| flaky appearance | | flaky appearance | ||
| usu. none req., p63+, HMWK+ | | usu. none req., p63+, HMWK+ | ||
| [[keratoacanthoma]], [[Paget disease]] | | [[keratoacanthoma]], [[Paget disease]] ([[EMPD]] & [[PDB]]), [[malignant melanoma]], Toker cell hyperplasia | ||
| Other | | Other | ||
| [ | | [[Image:Oral_cancer_%281%29_squamous_cell_carcinoma_histopathology.jpg|thumb|center|150px|SCC (WC)]] | ||
|- | |- | ||
| [[Malignant melanoma]] | | [[Malignant melanoma]] | ||
| | | spindle and/or epithelioid morphology +/-nuclear atypia (esp. nucleoli) | ||
| mitoses (esp. deep), +/-pigment, +/-nested arch., asymmetry, upward spread (into epidermis), epithelioid m. deep | | mitoses (esp. deep), +/-pigment, +/-nested arch., asymmetry, upward spread (into epidermis), epithelioid m. deep, +/-single cells, +/-sheets of cells | ||
| ABCD = Asymmetry, Borders poor demarc., Colour dark, Diameter large | | ABCD = Asymmetry, Borders poor demarc., Colour dark, Diameter large | ||
| S100+, Melan A+, HMB-45+, microphthalmia+, tyrosinase+ | | S100+, Melan A+, HMB-45+, microphthalmia+, tyrosinase+ | ||
| [[melanocytic lesions]] | | [[melanocytic lesions]] esp. [[Spitz nevus]], [[Bowen's disease]] | ||
| may be familial, [[dysplastic nevus]] | | may be familial, [[dysplastic nevus]] | ||
| [ | | [[Image:Malignant_melanoma_%281%29_at_thigh_Case_01.jpg |thumb|center|150px|Melanoma (WC)]] | ||
|- <!-- | |- <!-- | ||
| Entity | | Entity | ||
| Line 480: | Line 650: | ||
| [[hyaline globules]] (intracytoplasmic) | | [[hyaline globules]] (intracytoplasmic) | ||
| often HIV/AIDS | | often HIV/AIDS | ||
| HHV-8 | | [[HHV-8]] | ||
| [[Masson's hemangioma]], [[angiosarcoma]] | | [[Masson's hemangioma]], [[angiosarcoma]], [[Kaposiform hemangioendothelioma]] | ||
| | | stages: patch stage, plaque stage, nodular stage, exophytic, infiltrative, lymphadenopathic | ||
| [ | | [[Image:Kaposi_sarcoma_low_intermed_mag.jpg |thumb|center|150px| Kaposi sarcoma (WC)]] | ||
|- | |- | ||
| [[Cutaneous T-cell lymphoma]] (mycosis fungoides) | | [[Cutaneous T-cell lymphoma]] (includes ''mycosis fungoides'') | ||
| single lymphocytes in epidermis ("lymphocyte exocytosis") | | single lymphocytes in epidermis ("lymphocyte exocytosis") | ||
| lymphocyte nests in the epidermis ("Pautrier microabscesses"), short arrays of lymphocytes along the basal layer of the epidermis ("epidermotropism") | | lymphocyte nests in the epidermis ("Pautrier microabscesses"), short arrays of lymphocytes along the basal layer of the epidermis ("epidermotropism") | ||
| Line 492: | Line 662: | ||
| B cell lymphoma (?) | | B cell lymphoma (?) | ||
| Other | | Other | ||
| [ | | [[Image:Cutaneous_T-cell_lymphoma_-_intermed_mag.jpg |thumb|center|150px| CTCL (WC)]] | ||
|- | |- | ||
| [[Atypical fibroxanthoma]] | | [[Atypical fibroxanthoma]] | ||
| Line 501: | Line 671: | ||
| sarcomatoid squamous carcinoma, [[melanoma]], [[leiomyosarcoma]] | | sarcomatoid squamous carcinoma, [[melanoma]], [[leiomyosarcoma]] | ||
| some classify this as '''benign'''; thought to be related to [[undifferentiated pleomorphic sarcoma]] | | some classify this as '''benign'''; thought to be related to [[undifferentiated pleomorphic sarcoma]] | ||
| [ | | [[Image:SkinTumors-P9280874.jpg|thumb|center|150px| AFX (WC)]] | ||
|- | |- | ||
| [[Merkel cell carcinoma]] | | [[Merkel cell carcinoma]] | ||
| Line 510: | Line 680: | ||
| cutaneous [[Ewing sarcoma]], [[basal cell carcinoma]], (dermal) [[lymphoma]], metastatic small cell carcinoma (e.g. [[Lung tumours#Small cell carcinoma|lung]]) | | cutaneous [[Ewing sarcoma]], [[basal cell carcinoma]], (dermal) [[lymphoma]], metastatic small cell carcinoma (e.g. [[Lung tumours#Small cell carcinoma|lung]]) | ||
| rare, aggressive | | rare, aggressive | ||
| [ | | [[Image:Merkel_cell_carcinoma_-_very_high_mag.jpg |thumb|center|100px| MCC (WC)]] | ||
|- | |- | ||
| [[Dermatofibrosarcoma protuberans]] (DFSP) | | [[Dermatofibrosarcoma protuberans]] (DFSP) | ||
| Line 519: | Line 689: | ||
| [[dermatofibroma]], [[solitary fibrous tumour]] (usu. deeper) | | [[dermatofibroma]], [[solitary fibrous tumour]] (usu. deeper) | ||
| rarely metastases, characteristic [[translocation]]: t(17;22)(q22;q15) COLA1/PDGFB; may transform to [[fibrosarcoma]] | | rarely metastases, characteristic [[translocation]]: t(17;22)(q22;q15) COLA1/PDGFB; may transform to [[fibrosarcoma]] | ||
| [ | | [[Image:Storiform_pattern_-_intermed_mag.jpg |thumb|center|150px| DFSP (WC)]] | ||
|- <!-- | |- <!-- | ||
| Entity | | Entity | ||
| Line 533: | Line 703: | ||
=Presentations= | =Presentations= | ||
==Leukoplakia== | ==Leukoplakia== | ||
{{Main|Leukoplakia}} | |||
DDx:<ref>{{Ref PBoD|1065}}</ref> | DDx:<ref>{{Ref PBoD|1065}}</ref> | ||
*Vitiligo (loss of pigment). | *Vitiligo (loss of pigment). | ||
*Inflammation. | *Inflammation. | ||
**Chronic dermatitis. | **Chronic dermatitis. | ||
**Psoriasis. | **[[Psoriasis]]. | ||
*Neoplasia. | *Neoplasia. | ||
**Vulvar intraepithelial neoplasia. | **[[Vulvar intraepithelial neoplasia]]. | ||
**[[Invasive_breast_cancer#Paget.27s_disease|Paget disease]]. | **[[Invasive_breast_cancer#Paget.27s_disease|Paget disease]]. | ||
**Invasive carcinoma. | **Invasive carcinoma. | ||
| Line 554: | Line 726: | ||
! Image | ! Image | ||
|- | |- | ||
| Acanthosis nigricans | | [[Acanthosis nigricans]] | ||
| diabetes mellitus, malignancy | | [[diabetes mellitus]], malignancy | ||
| basal cell hyperpigmentation, hyperkeratosis, prominent rete ridges | | basal cell hyperpigmentation, hyperkeratosis, prominent rete ridges | ||
| [http://dermatology.cdlib.org/149/reviews/acanthosisnigricans/higgins.html (cdlib.org)] | | [http://dermatology.cdlib.org/149/reviews/acanthosisnigricans/higgins.html (cdlib.org)] | ||
| Line 561: | Line 733: | ||
| [[Trichilemmoma]] | | [[Trichilemmoma]] | ||
| [[Cowden disease]] | | [[Cowden disease]] | ||
| | | "hyperkeratosis" | ||
| | | [http://ccr.cancer.gov/staff/images/9033_12822_Lee_1520.jpg (cancer.gov)]<ref>URL: [http://ccr.cancer.gov/staff/gallery.asp?profileid=12822 http://ccr.cancer.gov/staff/gallery.asp?profileid=12822]. Accessed on: 14 December 2011.</ref> | ||
|- | |- | ||
| [[Angiokeratoma]] | | [[Angiokeratoma]] | ||
| [[Fabry disease]] | | [[Fabry disease]] | ||
| | | hyperkeratosis + vessels in superficial dermis | ||
| | | [http://commons.wikimedia.org/wiki/File:Angiokeratoma_-_low_mag.jpg (WC)] | ||
|- | |- | ||
| [[Dermatitis herpetiformis]] | | [[Dermatitis herpetiformis]] | ||
| [[Celiac disease]] | | [[Celiac disease]] | ||
| subepidermal [[bullous disease]] | | subepidermal [[bullous disease]], papillary abscesses | ||
| | | [http://www.lampyris101.com/L101/gallery1/12_JPG.html (lampyris101.com)] | ||
|- | |- | ||
| [[Angiofibroma]] | | [[Angiofibroma]] | ||
| [[tuberous sclerosis]] | | [[tuberous sclerosis]] | ||
| | | fibrotic dermis + dilated blood vessels | ||
| | | [http://www.drdittmar.lu/images/sce/angiofibroma-s.jpg (drdittmar.lu)] | ||
|- | |||
| [[Sebaceous adenoma]] | |||
| [[Muir-Torre syndrome]] | |||
| abundant sebaceous glands with abn. arch. | |||
| [http://commons.wikimedia.org/wiki/File:Sebaceous_adenoma_-_low_mag.jpg (WC)] | |||
|- | |||
| [[Seborrheic keratosis]], multiple with explosive onset | |||
| Leser–Trélat sign (malignancy) | |||
| horn cysts, hyperkeratosis | |||
| [http://commons.wikimedia.org/wiki/File:IMG_1724.JPG gross (WC)], [http://commons.wikimedia.org/wiki/File:Seborrheic_keratosis_%281%29.jpg micro. (WC)] | |||
|- <!-- | |||
| Entity | |||
| Disease/syndrome | |||
| Key histologic feature | |||
| Image --> | |||
|} | |} | ||
==Acanthosis nigricans== | ==Acanthosis nigricans== | ||
Associated with: [[ | ===General=== | ||
Associated with: | |||
*[[Diabetes mellitus]].<ref>URL: [http://www.emedicine.com/derm/topic1.htm http://www.emedicine.com/derm/topic1.htm], URL: [http://dermatlas.med.jhmi.edu/derm/indexDisplay.cfm?ImageID=1943559504].</ref> | |||
*Malignancy.<ref name=Ref_PCPBoD8|596>{{Ref PCPBoD8|596}}</ref> | |||
===Microscopic=== | ===Microscopic=== | ||
Features ''BPH'':<ref name=Ref_PCPBoD8|596>{{Ref PCPBoD8|596}}</ref> | Features (memory device ''BPH''):<ref name=Ref_PCPBoD8|596>{{Ref PCPBoD8|596}}</ref> | ||
*Basal cell hyperpigmentation. | *Basal cell hyperpigmentation. | ||
*Prominent rete ridges. | *Prominent rete ridges. | ||
*Hyperkeratosis. | *Hyperkeratosis. | ||
DDx: | |||
*[[Seborrheic keratosis]] - typically has more hyperkeratosis, pseudohorn cysts. | |||
Images: | Images: | ||
| Line 593: | Line 786: | ||
==Others== | ==Others== | ||
*[[Dermatitis herpetiformis]]: gluten enteropathy ([[celiac disease]]), [[thyroid]] disease, intestinal [[lymphoma]].<ref> | *[[Dermatitis herpetiformis]]: gluten enteropathy ([[celiac disease]]), [[thyroid]] disease, intestinal [[lymphoma]].<ref name=Ref_TN2007_D23>{{Ref TN2007|D23}}</ref> | ||
*[[Pemphigus vulgaris]]: [[thymoma]], myasthenia gravis, malignancy.<ref> | *[[Pemphigus vulgaris]]: [[thymoma]], myasthenia gravis, malignancy.<ref name=Ref_TN2007_D23>{{Ref TN2007|D23}}</ref> | ||
===Lipoid proteinosis=== | |||
<gallery> | |||
File:3767 dp sl 1.png |Lipoid proteinosis (A) | |||
File:3767 dp sl 2.png |Lipoid proteinosis (B) | |||
</gallery> | |||
A. Inner labial biopsy shows subepithelial hyalinized pink/red material, about blood vessels and in general. B. The particularly glassy appearance of the material in areas is evident at high power. | |||
===Xanthogranuloma in scrotal skin.=== | |||
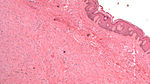
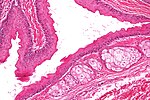
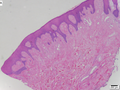
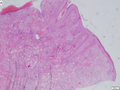
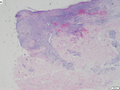
<gallery> | |||
File:DP16MR17 sl 1.png| Xanthogranuloma in scrotal skin. (A) | |||
File:DP16MR17 sl 2.png| Xanthogranuloma in scrotal skin. (B) | |||
File:DP16MR17 sl 3.png| Xanthogranuloma in scrotal skin. (C) | |||
File:DP16MR17 sl 4.png| Xanthogranuloma in scrotal skin. (D) | |||
</gallery> | |||
A. Pseudoepitheliomatous hyperplasia seemingly forms a dermal mass. B. Parakeratosis tops epidermis. C. Neutrophils lie in the center of the apparent mass. D. Diagnostic xanthoma cells lie in dermal papillae. | |||
===Silicone granuloma=== | |||
<gallery> | |||
File:DP13AP17 sl1.png| Silicone granuloma (A) | |||
File:DP13AP17 sl2.png| Silicone granuloma (B) | |||
File:DP13AP17 sl3.png| Silicone granuloma (C) | |||
File:DP13AP17 sl4.png| Silicone granuloma (D) | |||
</gallery> | |||
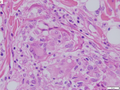
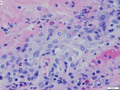
A. The dermis resembles Swiss cheese. B. Macrophages, some with more than one nucleus, accompany empty ovoid spaces. C. Some macrophages resemble Teuton body giant cells. D. An admixture of lymphocytes is not at all unusual. | |||
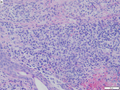
====Histoplasmosis in skin==== | |||
<gallery> | |||
File:DP20AP17 sl 1.png| Dermal histoplasmosis (A) | |||
File:DP20AP17 sl 2.png| Dermal histoplasmosis (B) | |||
File:DP20AP17 sl 3.png| Dermal histoplasmosis (C) | |||
File:DP20AP17 sl 4.png| Dermal histoplasmosis (D) | |||
</gallery> | |||
A. Extending from papillary dermis into dermis is a chronic, blue inflammatory infiltrate. B. The infiltrate comprises lymphocytes, plasma cells, and macrophages. C. At the edge of the biopsy pink strews inflammatory cells; this pink invasion of inflammation, so to speak, is a good place to look for organisms. D. High power reveals sometimes budding yeast forms in clear spaces. | |||
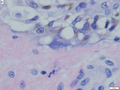
===Herpes Zoster=== | |||
<gallery> | |||
File:5.049889044 sl 1.png| Changes of herpes zoster (A) | |||
File:5.049889044 sl 2.png| Changes of herpes zoster (B) | |||
File:5.049889044 sl 3.png| Changes of herpes zoster (C) | |||
File:5.049889044 sl 4.png| Changes of herpes zoster (D) | |||
</gallery> | |||
Changes of herpes zoster in lower right abdominal skin of a 48 yo Hispanic man. A. Note the edema at the dermoepidermal junction along with a focal separation at the left as well as the inflamed superficial and deep blood vessels. B,C. Careful examination along the junction uncovers smudged chromatin diagnostic of viral infection. D. Vasculitis associated changes include extravasated neutrophils with nuclear dust, as well as pervascular macrophages, lymphocytes and occasional eosinophils. | |||
=References= | =References= | ||
Latest revision as of 20:38, 21 February 2020
Dermatopathology is the pathology of skin.
Pathology is a significant part of dermatology and dermatologists spend five years in residency. So, it is a huge area.
Specimens
- Shave biopsy = done for what is presumed to be benign disease - classically exophytic lesions, e.g. seborrheic keratosis.
- Saucerization = scooped shave biopsy.[1]
- Punch biopsy = cylindrical piece of skin, usu. epidermis and dermis - suspicious lesions/malignant lesions, e.g. basal cell carcinoma.
- Incisional biopsy = a piece of the lesion for pathologic assessment; lesion not completely removed.
- Excision = lesion cut-out with intent for complete removal - usual has a generous margin, e.g. malignant melanoma excision.
- Re-excision = done to get a wider margin or remove part of a lesion that was incompletely removed in a prior excision.
- Conservative re-excision = cut-out more with a minimal rim of normal tissue.[2]
- Sentinel lymph node removal = a special type of lymphadenectomy usu. done for staging, esp. malignant melanoma.
Histology
Layers of the skin
- Epidermis - outer most layer, avascular, separated from dermis by a basement membrane, epithelial tissue.
- Dermis - below the epidermis, vascular, separated from the epidermis by a basement membrane, connective tissue.
Note:
- The layer below the skin is the subdermis (AKA hypodermis, AKA subcutaneous tissue).
- It is below the dermis and consists of adipose tissue.[3]
Image:
Epidermis
Layers of the epidermis
Epidermis layers - from the surface to epidermal-dermal junction:
- Stratum corneum.
- Stratum lucidum.
- Present only in "thick" skin.[4]
- Stratum granulosum.
- Stratum spinosum (aka prickle layer).
- Stratum basale (germinativum).
Mnemonic: Corn Lovers Grow Several Bales.
Cells of the epidermis
- Keratinocytes.
- Usually eosinophilic cytoplasm - important feature.
- May have clear perinuclear halo (glycogenated keratinocytes).
- Intercellular bridges (high power) - key feature.
- Melanocytes.
- Usuallly basal location.
- Epithelioid or dendritic morphology.
- Pericellular clearing - key feature.
- Clear cytoplasm.
- +/-Pigmentation.
- Other:
- Toker cell.
- Neutrophils.
- Trilobated nuclei - 2-3 little dots - key feature.
- Lymphocytes.
- Small (round) nucleus.
- Scant/indistinct cytoplasm.
- Other foreign cells:
- Paget disease: large cells with clear cytoplasm, may cluster, above basal layer.
Normal histology
Features:
- Keratinocytes:
- Basal ~ 2x RBC.
- May palisade focally ~ 1:2 = width: height.
- Basal ~ 2x RBC.
- Melanocytes < 25 melanocytes / 0.5 mm of basal layer.[5]
- Basket weave stratum corneum (non-acral skin).
Dermis
Subdivided into layers:
- Papillary dermis.
- Location: superficial - opposed to the deep aspect of the epidermis.
- Appearance: dense, thick collagen bundles.
- Reticular dermis.
- Location: deep - between papillary dermis and subdermis.
- Appearance: loose connective tissue.
Images:
- Layers of the dermis - labelled (biology-online.org).[6]
- Layers of the skin (melanoma.blogsome.com).[7]
Adnexal structures
The top five structures of the skin:[8]
| Structure / Attribute | Histomorphology | Function | IHC | Other | Image |
|---|---|---|---|---|---|
| Eccrine gland | clusters of tubular structures, pale cytoplasm | thermoregulation (cooling) - produce sweat | CK7+, CEA+, CAM5.2+, EMA+ | ? | ? |
| Apocrine gland | apical snouts, tubular structures | ear wax, body odor | ? | ? | ? |
| Sebaceous gland | clusters of cells side-by-side, pale fluffy cytoplasm | grease hair, sexual lubrication | ? | assoc. with hair follicle | ? |
| Hair follicle | linear structure | keep individual warm | ? | assoc. with sebaceous glands | ? |
| Nail | epidermal structure | weapon (claw-like), look pretty? | ? | ? | (osumc.edu), (ctrgenpath.net) |
Ducts vs. glands:[9]
- Eccrine glands - spindle-shaped myoepithelial cells surround luminal cells.
- Eccrine ducts - cuboidal type subepithelial cells.
Common terms
Clinical descriptors
There are multitude of clinical descriptors - common ones are:[10]
| Name | Size † | Description | Other | Image |
|---|---|---|---|---|
| Macule | <= 10 mm | flat + change of colour | if > 10 mm --> patch | |
| Patch | > 10 mm | flat + change of colour | if <= 10 mm --> macule | |
| Papule | <= 10 mm | raised | if > 10 mm --> nodule | |
| Nodule | > 10 mm | raised | if <= 10 mm --> papule | |
| Plaque | > 10 mm | raised, flat-top | plateau-like | |
| Vesicle | <= 10 mm | raised, fluid filled | if > 10 mm --> bulla | |
| Bulla | > 10 mm | raised, fluid filled | if <= 10 mm --> vesicle |
Note:
- † Definitions vary -- some authors use a 5 mm cut-off.
Histologic descriptors
Dermatopathology doesn't have intuitive terms, e.g. thickening of the stratum spinosum isn't spinosum hyperplasia. The terms have to committed to memory.
Common terms in a table
| Term | Meaning | Reference |
|---|---|---|
| Acanthosis | thickening of the prickle layer (stratum spinosum) of epidermis | [11] |
| Acantholysis | loss of intercellular connections in the epidermis | |
| Dyskeratosis | abnormal keratinization, often refers to keratinization below the stratum granulosum; keratinization above may be abnormal (dependent on body site) | |
| Parakeratosis | retention of nuclei in the stratum corneum, normal in mucous membranes | |
| Spongiosis | epidermal intercellular edema; cells appear to have a clear halo around 'em | [12] |
| Basketweave stratum corneum | appearance of the normal stratum corneum; presence in the context of pathology suggests an acute process | |
| Compact hyperkeratosis | stratum corneum layer is dense and thickened; this suggests a chronic process | [13] |
| Hyperkeratosis | thickened stratum corneum - also see compact hyperkeratosis and basketweave stratum corneum | |
| Epidermotropism † | intraepithelial lymphocytes in CTCL; how to remember: epidermotropism = malignant | [14] |
| Exocytosis † | intraepithelial lymphocytes in benign conditions | [14] |
| Orthokeratosis | anuclear keratin layer is present (stratum corneum) - seen in normal skin; ortho- means correct | [15][16] |
Note:
- † These definitions are not universally accepted. Epidermotropism is sometimes used in the context of benign disease.[17]
Image:
Others terms
- Crust = epithelial elements, blood.
Image:
Skin diseases
Neoplasms
Malignant
Skin cancer is very common. The basic DDx of a malignant skin lesion is:
- Squamous cell carcinoma (SCC).
- Basal cell carcinoma (BCC).
- Malignant melanoma.
- Metastases.
Non-malignant disease
Non-malignant skin disease is common. It is the domain of dermatologists. It can be scary for general anatomical pathologists because the differential diagnosis is often broad, and, it's generally not something the general anatomical pathologist sees a lot of.
Subarticles
- Dermal cysts, e.g. epidermal cyst, pilar cyst.
- Epidermal necrosis, e.g. erythema multiforme, toxic epidermal necrolysis.
- Inflammatory skin diseases.
Common entities in tables
Non-malignant non-cystic - very common
| Entity | Key histologic feature | Other features | Clinical | Stains/IHC | DDx | Other | Image |
|---|---|---|---|---|---|---|---|
| Seborrheic keratosis (SK) | horn cysts (intraepidermal collections of keratin) | hyperkeratosis, brown granular material at the DE junction, sharply demarcated | stuck on appearance | none | fibroepithelial polyp | Leser–Trélat sign = many SKs in malignancy | |
| Dermatofibroma | fibrous bundles esp. at edge of lesion | "dirty fingers" = acanthosis + basal keratinocyte hyperpigmentation | +/-trauma Hx | CD34-, Factor XIIIa+ | DFSP | very common | |
| Fibroepithelial polyp (skin tag) | on a stalk (epithelium on 3+ sides) | no horn nests, no hyperkeratosis | raised lesion | none | seborrheic keratosis | very common | |
| Lipoma | mature adipocytes - uniform size | var. of size may be seen, should prompt search for lipoblasts | mobile subcutaneous mass | S100 (???) | liposarcoma | variants: angiolipoma (blood vessels), myolipoma (muscle) | |
| Cicatrix (dermal scar) | dense collagen bundles running parallel to DE junction, loss of dermal papillae | loss of adnexal structures, +/-giant cells, +/-foreign material, +/-inflammatory cells | site of previous trauma/surgery | usu. none; S-100 (to exclude melanoma) | residual disease, hypertrophic scar, (desmoplastic) melanoma |
Non-malignant non-cystic - common
| Entity | Key histologic feature | Other features | Clinical | Stains/IHC | DDx | Other | Image |
|---|---|---|---|---|---|---|---|
| Neurofibroma | bland spindle cells | mast cells, mixed with collagen, assoc. with a nerve | may be associated with neurofibromatosis, esp. plexiform type | S100+, GFAP+ | neurotized melanocytic nevus | may develop into MPNST | |
| Keratoacanthoma | keratin plug, glassy pink cytoplasm, pushing downward growth | minimal/no nuclear atypia | grow rapidly then involute | none | squamous cell carcinoma | some don't believe in the entity | |
| Molluscum contagiosum | suprabasilar cells with abundant granular eosinophilic cytoplasm | small peripheral nucleus | polypoid lesion; mushroom-like (?) | none (?) | DDx (?) | favourite exam case | |
| Verruca vulgaris | hypergranulosis (thick granular layer) + keratohyaline granules | hyperkeratosis (thick s. corneum), acanthosis (thick s. spinosum), rete ridges lengthened (~7-10x normal), large vessels at DE junction, koilocytic change (???) | raised lesions, classically on hand | none (p16+?) | squamous cell carcinoma | caused by HPV | |
| Condyloma acuminatum | koilocytes | parakeratosis, long folded rete ridges (papillomatosis) - pseudopapillary look | genital lesion | none (p16+) | fibroepithelial polyp | caused by HPV | |
| Granuloma annulare | dermal palisading granuloma around necrotic collagen | mucin in centre of lesion, (peripheral) lymphocytes, usu. more superficial than necrobiosis lipoidica | benign, self-limited | none (CD68?) | necrobiosis lipoidica, rheumatoid nodule, epithelioid sarcoma | Other ? | |
| Necrobiosis lipoidica | dermal palisading granuloma around necrotic collagen, plasma cells | mucin in centre of lesion, (peripheral) chronic inflammatory cells | may be assoc. diabetes mellitus | none (CD68?) | granuloma annulare, rheumatoid nodule | histology identical to necrobiosis lipoidica diabeticorum | (drmihm.com) |
| Angiofibroma | fibrotic dermis, dilated capillaries | enlarged (stellate fibroblasts) | dome-shaped - face, boys & nosebleeds (nasopharyngeal angiofibroma) | Stains/IHC | DDx | may be associated with tuberous sclerosis | |
| Keloid | thick collagen bundles - surrounded by paler staining fibroblasts | replaces adnexal structures | site of previous trauma, esp. in blacks | none | dermatofibroma (???) | hypertrophic scar | |
| Eccrine poroma | abundant basaloid cells with (small) ductal structures | incloses islands of sclerotic stroma with edema | erythematous lesions | Stains/IHC ? | DDx ? | Other ? | |
| Syringoma | bilayered ducts, occasionally tadpole like shape | usu. close to eyelid | Stains/IHC ? | DDx ? | Other ? | (cdlib.org) | |
| Chondroid syringoma (mixed tumour of skin) | chondromyxoid stroma, epithelial component | epithelial component in nests with eosinophilic cytoplasm, round/ovoid nuclei with nucleoli | Clinical ? | Stains/IHC ? | DDx ? | related to pleomorphic adenoma (???) | Image ? |
| Angiokeratoma | ectatic superficial dermal vessels + overlying hyperkeratosis | - | may be seen in Fabry disease | Stains/IHC ? | venous lake | Other ? |
Non-malignant non-cystic - children
| Entity | Key histologic feature | Other features | Clinical | Stains/IHC | DDx | Other | Image |
|---|---|---|---|---|---|---|---|
| Pilomatricoma | anucleate squamous cells (ghost cells), giant cells | bland basaloid cells | common in children | none | squamous cell carcinoma | mutations of CTNNB1 gene | |
| Juvenile xanthogranuloma (JXG) | Touton giant cells - multi-nucleated cells where nuclei are distributed around the cell periphery forming a ring | abundant cytoplasm | children | CD68+, CD1a-, CD207- | Langerhans cell histiocytosis | may be seen in adults, known as adult xanthogranuloma |
Non-malignant cystic
| Entity | Key histologic feature | Other features | Clinical | Stains/IHC | DDx | Other | Image |
|---|---|---|---|---|---|---|---|
| Epidermal cyst | cyst lined by squamous epithelium with a granular layer | keratinous debris, no skin adnexal structures | cyst | none | pilar cyst, dermoid cyst | Other? | |
| Pilar cyst (trichilemmal cyst) | cyst lined by squamous epithelium without a granular layer | keratinous debris | cyst | none | epidermal cyst | Other? | |
| Steatocystoma | cyst lined by squamous epithelium with a corrugated eosinophilic lining | epidermis has no granular layer | cyst | none | dermoid cyst, follicular cyst | Other? | |
| Dermoid cyst | cyst lined by keratinizing squamous epithelium with adnexal structures | adnexal structure = hair, sebaceous gland, sweat glands | cyst | none | epidermal cyst | may be seen in the ovary | (uiowa.edu) |
Pre-malignant
| Entity | Key histologic feature | Other features | Clinical | Stains/IHC | DDx | Other | Image |
|---|---|---|---|---|---|---|---|
| Actinic keratosis | epidermal atypia, esp. (basal) nuclear enlargement | var. of nuclear size, shape and staining, parakeratosis (important in early lesions); does not involves adnexal epithelium and follicular epithelium | yellow-brown scaly | none | squamous carcinoma, Bowen disease | seen with solar elastosis | |
| Bowen disease (squamous cell carcinoma in situ) | epidermal atypia, esp. suprabasal nuclear enlargement | var. of nuclear size, shape and staining; usually full thickness involvement; involve adnexal epithelium and follicular epithelium | none | squamous carcinoma, actinic keratosis | typically seen with solar elastosis |
Common malignant
| Entity | Key histologic feature | Other features | Clinical | Stains/IHC | DDx | Other | Image |
|---|---|---|---|---|---|---|---|
| Basal cell carcinoma (BCC) | basaloid cells with peripheral palisading, artificial cleft | myxoid stroma | raised, pearly, telangiectasia | usu. none req., CK5/6+ | trichoepithelioma, basaloid squamous cell carcinoma | assoc. nevoid basal cell carcinoma syndrome, Bazex syndrome | |
| Squamous cell carcinoma (SCC) | nuclear enlargement, eosinophilic cytoplasm, central nucleus | small nucleolus, intercellular bridges | flaky appearance | usu. none req., p63+, HMWK+ | keratoacanthoma, Paget disease (EMPD & PDB), malignant melanoma, Toker cell hyperplasia | Other | |
| Malignant melanoma | spindle and/or epithelioid morphology +/-nuclear atypia (esp. nucleoli) | mitoses (esp. deep), +/-pigment, +/-nested arch., asymmetry, upward spread (into epidermis), epithelioid m. deep, +/-single cells, +/-sheets of cells | ABCD = Asymmetry, Borders poor demarc., Colour dark, Diameter large | S100+, Melan A+, HMB-45+, microphthalmia+, tyrosinase+ | melanocytic lesions esp. Spitz nevus, Bowen's disease | may be familial, dysplastic nevus |
Less common malignant
| Entity | Key histologic feature | Other features | Clinical | Stains/IHC | DDx | Other | Image |
|---|---|---|---|---|---|---|---|
| Kaposi sarcoma | vascular spindle cell lesion | hyaline globules (intracytoplasmic) | often HIV/AIDS | HHV-8 | Masson's hemangioma, angiosarcoma, Kaposiform hemangioendothelioma | stages: patch stage, plaque stage, nodular stage, exophytic, infiltrative, lymphadenopathic | |
| Cutaneous T-cell lymphoma (includes mycosis fungoides) | single lymphocytes in epidermis ("lymphocyte exocytosis") | lymphocyte nests in the epidermis ("Pautrier microabscesses"), short arrays of lymphocytes along the basal layer of the epidermis ("epidermotropism") | Clinical | CD45, CD4 | B cell lymphoma (?) | Other | |
| Atypical fibroxanthoma | dermal lesion with marked nuclear atypia | multinucleated cells, mitoses, vacuolated cytoplasm | old men, head and neck | p63-, 34betaE12-, S100-, desmin- | sarcomatoid squamous carcinoma, melanoma, leiomyosarcoma | some classify this as benign; thought to be related to undifferentiated pleomorphic sarcoma | |
| Merkel cell carcinoma | neuroendocrine nuclear features (stippled chromatin, no nucleolus), scant cytoplasm | +/-nuclear moulding, usu. intermediate cell size | Merkel cell polyomavirus associated, usu. head & neck or extremities | CK20+, EMA+ | cutaneous Ewing sarcoma, basal cell carcinoma, (dermal) lymphoma, metastatic small cell carcinoma (e.g. lung) | rare, aggressive | |
| Dermatofibrosarcoma protuberans (DFSP) | spindle cell tumour with storiform pattern, tumour often contains adipocytes | dermal tumour with preserved adnexal structures | locally aggressive | CD34+, factor XIIIa- | dermatofibroma, solitary fibrous tumour (usu. deeper) | rarely metastases, characteristic translocation: t(17;22)(q22;q15) COLA1/PDGFB; may transform to fibrosarcoma |
Presentations
Leukoplakia
DDx:[19]
- Vitiligo (loss of pigment).
- Inflammation.
- Chronic dermatitis.
- Psoriasis.
- Neoplasia.
- Vulvar intraepithelial neoplasia.
- Paget disease.
- Invasive carcinoma.
- Other.
Skin disease and systemic conditions
Tabular list
| Entity | Disease/syndrome | Key histologic feature | Image |
|---|---|---|---|
| Acanthosis nigricans | diabetes mellitus, malignancy | basal cell hyperpigmentation, hyperkeratosis, prominent rete ridges | (cdlib.org) |
| Trichilemmoma | Cowden disease | "hyperkeratosis" | (cancer.gov)[20] |
| Angiokeratoma | Fabry disease | hyperkeratosis + vessels in superficial dermis | (WC) |
| Dermatitis herpetiformis | Celiac disease | subepidermal bullous disease, papillary abscesses | (lampyris101.com) |
| Angiofibroma | tuberous sclerosis | fibrotic dermis + dilated blood vessels | (drdittmar.lu) |
| Sebaceous adenoma | Muir-Torre syndrome | abundant sebaceous glands with abn. arch. | (WC) |
| Seborrheic keratosis, multiple with explosive onset | Leser–Trélat sign (malignancy) | horn cysts, hyperkeratosis | gross (WC), micro. (WC) |
Acanthosis nigricans
General
Associated with:
- Diabetes mellitus.[21]
- Malignancy.[22]
Microscopic
Features (memory device BPH):[22]
- Basal cell hyperpigmentation.
- Prominent rete ridges.
- Hyperkeratosis.
DDx:
- Seborrheic keratosis - typically has more hyperkeratosis, pseudohorn cysts.
Images:
Others
- Dermatitis herpetiformis: gluten enteropathy (celiac disease), thyroid disease, intestinal lymphoma.[23]
- Pemphigus vulgaris: thymoma, myasthenia gravis, malignancy.[23]
Lipoid proteinosis
A. Inner labial biopsy shows subepithelial hyalinized pink/red material, about blood vessels and in general. B. The particularly glassy appearance of the material in areas is evident at high power.
Xanthogranuloma in scrotal skin.
A. Pseudoepitheliomatous hyperplasia seemingly forms a dermal mass. B. Parakeratosis tops epidermis. C. Neutrophils lie in the center of the apparent mass. D. Diagnostic xanthoma cells lie in dermal papillae.
Silicone granuloma
A. The dermis resembles Swiss cheese. B. Macrophages, some with more than one nucleus, accompany empty ovoid spaces. C. Some macrophages resemble Teuton body giant cells. D. An admixture of lymphocytes is not at all unusual.
Histoplasmosis in skin
A. Extending from papillary dermis into dermis is a chronic, blue inflammatory infiltrate. B. The infiltrate comprises lymphocytes, plasma cells, and macrophages. C. At the edge of the biopsy pink strews inflammatory cells; this pink invasion of inflammation, so to speak, is a good place to look for organisms. D. High power reveals sometimes budding yeast forms in clear spaces.
Herpes Zoster
Changes of herpes zoster in lower right abdominal skin of a 48 yo Hispanic man. A. Note the edema at the dermoepidermal junction along with a focal separation at the left as well as the inflamed superficial and deep blood vessels. B,C. Careful examination along the junction uncovers smudged chromatin diagnostic of viral infection. D. Vasculitis associated changes include extravasated neutrophils with nuclear dust, as well as pervascular macrophages, lymphocytes and occasional eosinophils.
References
- ↑ Elston, D. (Jul 2012). "Practical advice regarding problematic pigmented lesions.". J Am Acad Dermatol 67 (1): 148-55. doi:10.1016/j.jaad.2012.04.006. PMID 22703907.
- ↑ URL: http://www.nedermatology.com/skin-cancer-treatments.php. Accessed on: 26 February 2013.
- ↑ URL: http://histologyolm.stevegallik.org/node/119. Accessed on: 5 November 2013.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 1. ISBN 978-0443066542.
- ↑ Trotter, MJ. (Jun 2011). "Melanoma margin assessment.". Clin Lab Med 31 (2): 289-300. doi:10.1016/j.cll.2011.03.006. PMID 21549242.
- ↑ URL: http://www.biology-online.org/articles/fibroblast_heterogeneity_skin_deep/figures.html. Accessed on: 29 March 2012.
- ↑ URL: http://melanoma.blogsome.com/category/skin-structure/. Accessed on: 29 March 2012.
- ↑ Busam, Klaus J. (2009). Dermatopathology: A Volume in the Foundations in Diagnostic Pathology Series (1st ed.). Saunders. pp. 4-8. ISBN 978-0443066542.
- ↑ HJ. 27 Feb 2009.
- ↑ URL: http://www.pediatrics.wisc.edu/education/derm/text.html. Accessed on: 18 September 2012.
- ↑ http://dictionary.reference.com/browse/acanthosis
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1230. ISBN 0-7216-0187-1.
- ↑ URL: http://dermnetnz.org/pathology/pathology-glossary.html. Accessed on: 8 August 2012.
- ↑ 14.0 14.1 Fung, MA. (May 2010). "'Epidermotropism' vs. 'exocytosis' of lymphocytes 101: definition of terms.". J Cutan Pathol 37 (5): 525-9. doi:10.1111/j.1600-0560.2010.01515.x. PMID 20132423.
- ↑ URL: http://www.medilexicon.com/medicaldictionary.php?t=63448. Accessed on: 13 March 2013.
- ↑ URL: http://dictionary.reference.com/browse/ortho-. Accessed on: 13 March 2013.
- ↑ Fung, MA.; LeBoit, PE. (Apr 1998). "Light microscopic criteria for the diagnosis of early vulvar lichen sclerosus: a comparison with lichen planus.". Am J Surg Pathol 22 (4): 473-8. PMID 9537476.
- ↑ URL: http://www.eplasty.com/index.php?option=com_content&view=article&id=492&catid=171:volume-10-eplasty-2010&Itemid=121. Accessed on: 16 October 2012.
- ↑ Cotran, Ramzi S.; Kumar, Vinay; Fausto, Nelson; Nelso Fausto; Robbins, Stanley L.; Abbas, Abul K. (2005). Robbins and Cotran pathologic basis of disease (7th ed.). St. Louis, Mo: Elsevier Saunders. pp. 1065. ISBN 0-7216-0187-1.
- ↑ URL: http://ccr.cancer.gov/staff/gallery.asp?profileid=12822. Accessed on: 14 December 2011.
- ↑ URL: http://www.emedicine.com/derm/topic1.htm, URL: [1].
- ↑ 22.0 22.1 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 596. ISBN 978-1416054542.
- ↑ 23.0 23.1 Greenwald, J.; Heng, M. (2007). Toronto Notes for Medical Students 2007 (2007 ed.). The Toronto Notes Inc. for Medical Students Inc.. pp. D23. ISBN 978-0968592878.