Difference between revisions of "Embryonal carcinoma"
Jump to navigation
Jump to search
| Line 47: | Line 47: | ||
#Indistinct cell borders | #Indistinct cell borders | ||
#Mitoses - common. | #Mitoses - common. | ||
#Variable architecture: | #Variable architecture:<ref name=pmid24503753>{{Cite journal | last1 = Kao | first1 = CS. | last2 = Ulbright | first2 = TM. | last3 = Young | first3 = RH. | last4 = Idrees | first4 = MT. | title = Testicular embryonal carcinoma: a morphologic study of 180 cases highlighting unusual and unemphasized aspects. | journal = Am J Surg Pathol | volume = 38 | issue = 5 | pages = 689-97 | month = May | year = 2014 | doi = 10.1097/PAS.0000000000000171 | PMID = 24503753 }}</ref> | ||
#* | #*Solid (predominant in ~55% of cases). | ||
#*Glandular. | #*Glandular (predominant in ~17% of cases). | ||
#* | #*Papillary (predominant in ~11% of cases). | ||
#*Nested. | |||
#*Micropapillary. | |||
#*Anastomosing glandular. | |||
#*Sieve-like glandular. | |||
#*Pseudopapillary. | |||
#*Blastocyst-like. | |||
#*Embryoid bodies - ball of cells in surrounded by empty space on three sides. | #*Embryoid bodies - ball of cells in surrounded by empty space on three sides. | ||
Notes: | Notes: | ||
*Cytoplasmic staining variable (eosinophilic to basophilic). | *Cytoplasmic staining variable (eosinophilic to basophilic). | ||
*[[Syncytiotrophoblasts]] commonly seen (~40-50% of cases<ref name=pmid24503753/>). | |||
DDx: | DDx: | ||
*[[Mixed germ cell tumour]]. | *[[Mixed germ cell tumour]]. | ||
*[[Yolk sac tumour]]. | *[[Yolk sac tumour]]. | ||
*[[Seminoma]]. | |||
===Images=== | ===Images=== | ||
Revision as of 15:48, 26 November 2014
| Embryonal carcinoma | |
|---|---|
| Diagnosis in short | |
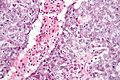
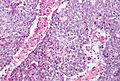
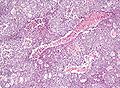
 Embryonal carcinoma. H&E stain. | |
|
| |
| LM | vesicular nuclei, nuclear overlap, necrosis (common), mitoses, variable architecture (tubulopapillary, glandular, solid, embryoid bodies) |
| LM DDx | seminoma, mixed germ cell tumour, yolk sac tumour, other carcinomas |
| IHC | OCT3 +ve, CD30 +ve, AE1/AE3 +ve, CD117 -ve |
| Site | testis, ovary, mediastinum |
|
| |
| Signs | testicular mass, pelvic mass |
Embryonal carcinoma is a type of germ cell tumour. It is commonly as a component of mixed germ cell tumours.
General
- Affects young adults.
- May be seen in women.
Gross
- Typically a testicular mass.
- May be seen in the mediastinum.[1]
Microscopic
Features:[2]
- Nucleoli - key feature.
- Vesicular nuclei (clear, empty appearing nuclei) - key feature.
- Nuclei overlap.
- Necrosis - common.
- Not commonly present in seminoma.
- Indistinct cell borders
- Mitoses - common.
- Variable architecture:[3]
- Solid (predominant in ~55% of cases).
- Glandular (predominant in ~17% of cases).
- Papillary (predominant in ~11% of cases).
- Nested.
- Micropapillary.
- Anastomosing glandular.
- Sieve-like glandular.
- Pseudopapillary.
- Blastocyst-like.
- Embryoid bodies - ball of cells in surrounded by empty space on three sides.
Notes:
- Cytoplasmic staining variable (eosinophilic to basophilic).
- Syncytiotrophoblasts commonly seen (~40-50% of cases[3]).
DDx:
Images
IHC
ISUP consensus
General panel:[4]
- OCT4 +ve.
- Choriocarcinoma, yolk sac tumour and spermatocytic seminoma all -ve.
- CD30 +ve.
- -ve in seminoma.
- CD117 -ve.[5]
- +ve in seminoma.
Additional notes
See also
References
- ↑ Yalçın, B.; Demir, HA.; Tanyel, FC.; Akçören, Z.; Varan, A.; Akyüz, C.; Kutluk, T.; Büyükpamukçu, M. (Oct 2012). "Mediastinal germ cell tumors in childhood.". Pediatr Hematol Oncol 29 (7): 633-42. doi:10.3109/08880018.2012.713084. PMID 22877235.
- ↑ Zhou, Ming; Magi-Galluzzi, Cristina (2006). Genitourinary Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 549. ISBN 978-0443066771.
- ↑ 3.0 3.1 Kao, CS.; Ulbright, TM.; Young, RH.; Idrees, MT. (May 2014). "Testicular embryonal carcinoma: a morphologic study of 180 cases highlighting unusual and unemphasized aspects.". Am J Surg Pathol 38 (5): 689-97. doi:10.1097/PAS.0000000000000171. PMID 24503753.
- ↑ Ulbright TM, Tickoo SK, Berney DM, Srigley JR (August 2014). "Best practices recommendations in the application of immunohistochemistry in testicular tumors: report from the international society of urological pathology consensus conference". Am. J. Surg. Pathol. 38 (8): e50–9. doi:10.1097/PAS.0000000000000233. PMID 24832161.
- ↑ 5.0 5.1 Lau, SK.; Weiss, LM.; Chu, PG. (Mar 2007). "D2-40 immunohistochemistry in the differential diagnosis of seminoma and embryonal carcinoma: a comparative immunohistochemical study with KIT (CD117) and CD30.". Mod Pathol 20 (3): 320-5. doi:10.1038/modpathol.3800749. PMID 17277761.
- ↑ 6.0 6.1 Iczkowski, KA.; Butler, SL.; Shanks, JH.; Hossain, D.; Schall, A.; Meiers, I.; Zhou, M.; Torkko, KC. et al. (Feb 2008). "Trials of new germ cell immunohistochemical stains in 93 extragonadal and metastatic germ cell tumors.". Hum Pathol 39 (2): 275-81. doi:10.1016/j.humpath.2007.07.002. PMID 18045648.
- ↑ Jacobsen, GK.; Nørgaard-Pedersen, B. (Sep 1984). "Placental alkaline phosphatase in testicular germ cell tumours and in carcinoma-in-situ of the testis. An immunohistochemical study.". Acta Pathol Microbiol Immunol Scand A 92 (5): 323-9. PMID 6209917.