Difference between revisions of "Pheochromocytoma"
(→Sign out: more) |
|||
| Line 162: | Line 162: | ||
==Sign out== | ==Sign out== | ||
Mete ''et al.''. created a synoptic report for these cases that may be used.<ref pmid24476517>{{cite journal |vauthors=Mete O, Tischler AS, de Krijger R, McNicol AM, Eisenhofer G, Pacak K, Ezzat S, Asa SL |title=Protocol for the examination of specimens from patients with pheochromocytomas and extra-adrenal paragangliomas |journal=Arch Pathol Lab Med |volume=138 |issue=2 |pages=182–8 |date=February 2014 |pmid=24476517 |pmc=3909881 |doi=10.5858/arpa.2012-0551-OA |url=}}</ref> The ''College of American Pathologists''' does ''not'' have a synoptic for these currently (September 2021).{{fact}} | |||
<pre> | <pre> | ||
Right Adrenal (Mass), Adrenalectomy: | Right Adrenal (Mass), Adrenalectomy: | ||
Revision as of 18:50, 21 September 2021
| Pheochromocytoma | |
|---|---|
| Diagnosis in short | |
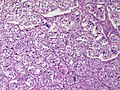
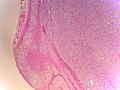
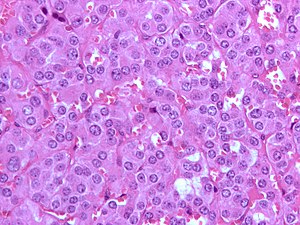 Pheochromocytoma. H&E stain. | |
|
| |
| LM | Zellballen (nests of cells), fibrovascular septae, salt-and-pepper nuclei, +/-hemorrhage (very common) |
| LM DDx | adrenocortical carcinoma, paraganglioma |
| IHC | chief cells: chromogranin A +ve, synaptophysin +ve; sustentacular cells: S-100 +ve |
| Site | adrenal gland (same tumour arising at other sites known as paraganglioma) |
|
| |
| Syndromes | Multiple endocrine neoplasia 2A and 2B, von Hippel-Lindau syndrome,Neurofibromatosis type 1, familial paraganglioma syndromes (several) |
|
| |
| Clinical history | hypertension (classic Hx), paroxysms of tachycardia, headache, anxiety, hypertension |
| Prevalence | uncommon |
| Prognosis | usually benign |
| Clin. DDx | other adrenal gland masses, renal cell carcinoma, other abdominal masses |
Pheochromocytoma is a tumour of the adrenal gland medulla. It may be benign or malignant.
General
- Considered to be a paraganglioma.[1]
- Literally means "dusky" (pheo) "colour" (chromo) - dull appearance on gross.
- Tumour arises from adrenal medulla - chromaffin cells.[2]
Memory device - the rule of 10s:[2]
- 10% extra-adrenal (e.g. carotid body, organ of Zuckerkandl (neighourhood of aortic bifuration/IMA branch point)).
- 10% bilateral.
- 10% malignant.
- 10% no hypertension.
- 25% associated within a syndrome:
- Multiple endocrine neoplasia 2A and 2B.
- von Hippel-Lindau syndrome.
- Neurofibromatosis type 1.
- Familial paraganglioma syndromes - several - see paraganglioma article.
Clinical
- Classic finding: hypertension.
- Paroxysms (i.e. episodes) of tachycardia, headache, anxiety, hypertension.
Laboratory findings (urine):
- Vanillylmandelic acid (VMA).
- Metanephrines.
Macroscopic
- Medullary tumour
- Round to oval mass
- Dusky red and possibly haemorrhagic
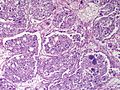
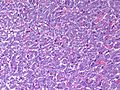
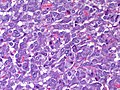
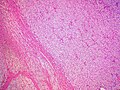
Microscopic
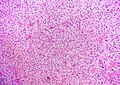
Features:[3]
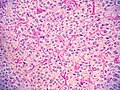
- Chief cells:
- Usu. polygonal cells, may be spindled.
- Arranged in cell nests - "Zellballen" (literally cell balls) - key feature.
- Stippled chromatin (AKA salt and pepper chromatin) - coarsely granular chromatin.
- Granular cytoplasm, often basophilic - important.
- Sustentacular cells (structural support cell).
- Often haemorrhagic - highly vascular.
- +/-Nuclear pleomorphism.
- Rarely pigmented [4]
Notes:
- The nested architecture (Zellballen) is useful for differentiating from ACC.
- Metastasis sole criteria of malignancy.[2]
- Surrounding adrenal cortex is typically compressed.[5]
DDx:
- Adrenal cortical carcinoma - pheochromocytoma versus adrenal cortical carcinoma.
- Paraganglioma - same lesion arising outside of the adrenal gland.
Images
Pheochromocytoma versus adrenal cortical carcinoma
- Pheochromocytoma and adrenal cortical carcinoma overlap histologically.[6]
Favour pheochromocytoma:
- Small chickenwire-pattern blood vessels, nests, salt-and-pepper chromatin, red blood cell extravasation.
Favour adrenal cortical carcinoma:
- Nucleolus, sheeting.
Malignant pheochromoctyoma
- Robbins (8th Ed.) says metastases are the sole criteria of malignancy.[2]
- Thompson suggests one can differentiate benign from malignant with the aid of the following:[7]
- Marked nuclear atypia.
- Invasion:
- Capsular.
- Vascular.
- Necrosis.
- Cellular monotony.
- Mitoses:
- Rate.
- Atypical mitosis.
IHC
- Chief cells:
- Chromogranin A +ve.
- Synaptophysin +ve.
- Sustentacular cells:
- S100 +ve.
Pheochromocytoma versus adrenal cortical carcinoma (ACC):[6]
- Melan A -ve.
- Positive in ACC.
- Inhibin -ve.
- Positive in ACC.
- Calretinin -ve.
- Positive in ACC.
A panel:
- S-100, chromogranin, calretinin, EMA, PAX8.
Electron microscopy
- Membrane-bound secretory granules.
Sign out
Mete et al.. created a synoptic report for these cases that may be used.Cite error: Invalid <ref> tag; invalid names, e.g. too many The College of American Pathologists' does not have a synoptic for these currently (September 2021).[citation needed]
Right Adrenal (Mass), Adrenalectomy:
- Pheochromocytoma, margin clear.
Comment:
The tumour stains as follows:
POSITIVE: synaptophysin, chromogranin A, S-100 (sustentacular cells).
NEGATIVE: EMA, inhibin.
Proliferation (Ki-67): <2% of tumour cells.
The immunostaining pattern is consistent with a pheochromocytoma.
Block letters
ADRENAL MASS, RIGHT, ADRENALECTOMY: - PHEOCHROMOCYTOMA. - SURGICAL MARGIN NEGATIVE FOR PHEOCHROMOCYTOMA. COMMENT: The tumour cells stains for chromogranin and synaptophysin. S-100 marks the sustentacular cells. Inhibin is negative in the tumour cells. The immunostaining pattern is consistent with a pheochromocytoma.
Micro
The sections shows a partially hemorrhagic lesion in the medulla of the adrenal gland that is arranged in nests (Zellballen). The tumour cells have abundant grey/blue granular cytoplasm, and nuclei with granular chromatin (salt and pepper chromatin). The lesion is surrounded by a compressed rim of adrenal cortex and fibrosis tissue. The core of the lesion is fibrotic and has clusters of hemosiderin-laden macrophages.
There is no capsular invasion. Vascular invasion is not identified. There is no necrosis. Mitotic activity is not appreciated.
The adrenal cortex is unremarkable.
See also
References
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 327. ISBN 978-0443066856.
- ↑ 2.0 2.1 2.2 2.3 Mitchell, Richard; Kumar, Vinay; Fausto, Nelson; Abbas, Abul K.; Aster, Jon (2011). Pocket Companion to Robbins & Cotran Pathologic Basis of Disease (8th ed.). Elsevier Saunders. pp. 586. ISBN 978-1416054542.
- ↑ Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson; Aster, Jon (2009). Robbins and Cotran pathologic basis of disease (8th ed.). Elsevier Saunders. pp. 1161. ISBN 978-1416031215.
- ↑ Bellezza, G.; Giansanti, M.; Cavaliere, A.; Sidoni, A. (Oct 2004). "Pigmented "black" pheochromocytoma of the adrenal gland: a case report and review of the literature.". Arch Pathol Lab Med 128 (10): e125-8. doi:10.1043/1543-2165(2004)128<e125:PBPOTA>2.0.CO;2. PMID 15387689.
- ↑ URL: http://www.pathpedia.com/Education/eAtlas/Histopathology/Adrenal/Pheochromocytoma.aspx. Accessed on: 27 May 2013.
- ↑ 6.0 6.1 Sangoi, AR.; McKenney, JK. (Mar 2010). "A tissue microarray-based comparative analysis of novel and traditional immunohistochemical markers in the distinction between adrenal cortical lesions and pheochromocytoma.". Am J Surg Pathol 34 (3): 423-32. doi:10.1097/PAS.0b013e3181cfb506. PMID 20154585.
- ↑ Thompson, Lester D. R. (2006). Endocrine Pathology: A Volume in Foundations in Diagnostic Pathology Series (1st ed.). Churchill Livingstone. pp. 259. ISBN 978-0443066856.