Thymoma
Jump to navigation
Jump to search
Thymoma is a common tumour of the thymus.
General
- Strong association with autoimmune disease, esp. myasthenia gravis.
Classification
The WHO published a widely used system - WHO classification:[1]
Type A
- AKA Spindle cell or medullary.
- Arise from medullary epithelial cells.
- Good prognosis.
IHC:
- Usu. keratin+.
Type AB
- Like Type A... but with foci of lymphocytes.
Type B1
- Near normal, expanded cortex.
Lesion consists of:
- >2/3 lymphocytes, <1/3 cortical epithelial cells.
Type B2
- Neoplastic cells with some resemblance to cortical epithelial cells.
- Epithelioid cells with distinct nucleoli.
- May be perivascular.
- Large population of lymphocytes.
Lesion consists of:
- <2/3 but >1/3 lymphocytes, >1/3 but <2/3 cortical epithelial cells.
Notes:
- Most common B type.
Type B3
- Neoplastic cells with some resemblance to cortical epithelial cells.
- Polygonal/round shape.
- Form sheets (of cells) - key feature.
- Lymphocytes - less than in Type B2.
- AKA well-differentiated thymic carcinoma.
Lesion consists of:
- <1/3 lymphocytes, >2/3 cortical epithelial cells.
Note:
- Neoplastic cells derived from the thymus with cytologic features of malignancy are thymic carcinomas.
Images:
Gross
- Light brown/tan.
- Encapsulated.
Image:
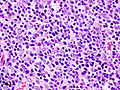
Microscopic
Features:
- Lymphocytes.
- Epithelial cells.
- Spindle cells - Type A.
- Epithelioid cells - Type B.
DDx:
Images:
Staging
There is a system by Masaoka and colleagues[2] that was subsequently modified, and is known as the modified Masaoka staging system.[3]
Based on CAP protocol
Staging as per Butnor et al.:[4]
| Stage | Characteristics |
|---|---|
| I | encapsulated lesion, tumour does not penetrate capsule |
| IIa | microscopic penetration of the capsule |
| IIb | macroscopic penetration of the capsule |
| III | macroscopic invasion of adjacent organs |
| IVa | pleural or pericardial spread |
| IVb | lymphatic or hematogenous spread |
Modified Masaoka as per Masaoka et al. (1999)
T-stage - based on Masaoka et al. (1999):[5]
| Stage | Features |
|---|---|
| T1 | macroscopically and microscopically encapulated |
| T2 | macroscopic invasion or adhesion to surrounding tissue (fat or pleura) or microscopic invasion into the capsule |
| T3 | Spread to adjacent organs, e.g. pericardium, lung, great vessels. |
| T4 | pericardial or pleural spread |
N-stage - based on Masaoka et al. (1999):[5]
| Stage | Features |
|---|---|
| N0 | no lymph node spread |
| N1 | spread to anterior mediastinal lymph nodes |
| N2 | spread to intrathoracic lymph nodes other than the mediastinal lymph nodes |
| N3 | spread to supraclavicular lymph nodes |
M-stage - based on Masaoka et al. (1999):[5]
| Stage | Features |
|---|---|
| M0 | no hematogeneous spread and extrathoracic lymph nodes with the exception of the supraclavicular nodes |
| M1 | hematogeneous spread and/or extrathoracic lymph nodes |
IHC
A panel:
- TdT, CD1a, CD3, CD5, CD20, Ki-67, CD117, p63, CK5/6.
Sign out
A. Lymph Node, Station 6, Lymphadenectomy: - One benign lymph node (0/1). B. Submitted as "Anterior Mediastinal Tumour (Thymus)", Excision: - Thymoma, WHO type B2. - Modified Masaoka stage IIa. - Three benign lymph nodes (0/3). - Rim of benign thymus. - Please see synoptic report.
See also
References
- ↑ Mills, Stacey E; Carter, Darryl; Greenson, Joel K; Oberman, Harold A; Reuter, Victor E (2004). Sternberg's Diagnostic Surgical Pathology (4th ed.). Lippincott Williams & Wilkins. pp. 1264. ISBN 978-0781740517.
- ↑ Masaoka, A.; Monden, Y.; Nakahara, K.; Tanioka, T. (Dec 1981). "Follow-up study of thymomas with special reference to their clinical stages.". Cancer 48 (11): 2485-92. PMID 7296496.
- ↑ Koga, K.; Matsuno, Y.; Noguchi, M.; Mukai, K.; Asamura, H.; Goya, T.; Shimosato, Y. (May 1994). "A review of 79 thymomas: modification of staging system and reappraisal of conventional division into invasive and non-invasive thymoma.". Pathol Int 44 (5): 359-67. PMID 8044305.
- ↑ Butnor KJ et al. Thymus. Version 3.1.0.0. 2011. URL: www.cap.org/cancerprotocols. Accessed on: 31 August 2015.
- ↑ 5.0 5.1 5.2 Masaoka, A.; Yamakawa, Y.; Fujii, Y. (Mar 1999). "Well-differentiated thymic carcinoma: is it thymic carcinoma or not?". J Thorac Cardiovasc Surg 117 (3): 628-30. PMID 10047676.
- ↑ Adam P, Hakroush S, Hofmann I, Reidenbach S, Marx A, Ströbel P (June 2014). "Thymoma with loss of keratin expression (and giant cells): a potential diagnostic pitfall". Virchows Arch.. doi:10.1007/s00428-014-1606-6. PMID 24923897.
- ↑ Viti, A.; Bertolaccini, L.; Cavallo, A.; Fortunato, M.; Bianchi, A.; Terzi, A. (Sep 2014). "18-Fluorine fluorodeoxyglucose positron emission tomography in the pretreatment evaluation of thymic epithelial neoplasms: a metabolic biopsy confirmed by Ki-67 expression.". Eur J Cardiothorac Surg 46 (3): 369-74; discussion 374. doi:10.1093/ejcts/ezu030. PMID 24585679.